70 years of progress in cervical cancer research

25 years ago, our scientists showed that nearly all cervical cancers are caused by the human papillomavirus (HPV). This discovery was a key step towards today’s vaccination programme and improvements made to the cervical cancer screening programme.
But that’s not where our story with cervical cancer research starts, and it certainly isn’t where it ends.
We’ve been at the heart of research into cervical cancer since the late 1950s. That’s 50 years before the Imperial Cancer Research Fund and the Cancer Research Campaign merged to form Cancer Research UK as we know it now.
So, let’s take a walk through our history in cervical cancer research and look back on the progress that we’ve made in beating it.
1958
We pioneered one of the earliest UK cervical screening studies
Our first step takes us back around 70 years.
In the 1950s, researcher Erica Wachtel analysed smear tests - samples of cells from the cervix - from 165 patients following treatment for gynaecological cancers (such as endometrial, ovarian and cervical).
She discovered that measuring oestrogen activity helped predict if these cancers, including cervical cancer, were responding to treatment and spot the early signs of the cancer returning.


A scientist at work in a lab at the Imperial Cancer Research Fund in the 1960's
A scientist at work in a lab at the Imperial Cancer Research Fund in the 1960's

1988
The NHS Cervical Screening Programme began
30 years after that study, the cervical screening programme is rolled out across the UK with computerised invites that meant all eligible women were being offered screening.
At that time, cervical screening looked for abnormal changes to cervical cells and aimed to pick up changes that could develop into cervical cancer if left untreated, early.
Within the first 25 years of the screening programme, the number of cervical cancer cases falls by a third.

1993
Our scientists show how vaccination can protect cows from the bovine equivalent of HPV
In the early 1990s, scientists discovered that exposure to HPV could lead to cervical cancer over time, thanks in part to research led by our former chief scientist, Professor Karen Vousden.
Thanks to that research, we knew that if we could prevent or cure infection with HPV, it could lead to a decrease in the number of cervical cancer cases.
A study led by scientists at our Beatson Institute, Glasgow, was the first to demonstrate an effective vaccine against a papillomavirus in cows.
In their landmark paper, the research team concluded: “We believe that similar strategies can be used for vaccination in humans.”


1999
We show that nearly all cervical cancers are caused by HPV
By 1995, the International Biology Study of Cervical Cancer (IBSCC) had analysed over 1,000 cervical cancer samples across 22 countries and their results found the DNA of HPV in 93% of them.
These findings pointed to HPV as the cause of more than 9 in 10 cases of cervical cancer.
But four years later, even that was revealed to be an underestimate. By reanalysing some of the samples collected by the IBSCC, another group of researchers we funded found that HPV had been present in 99.7% of cases.
The team described HPV as the one factor causing the highest percentage of a single cancer in the world.
These remarkable findings put the gears in motion for the development of the HPV vaccination programme.


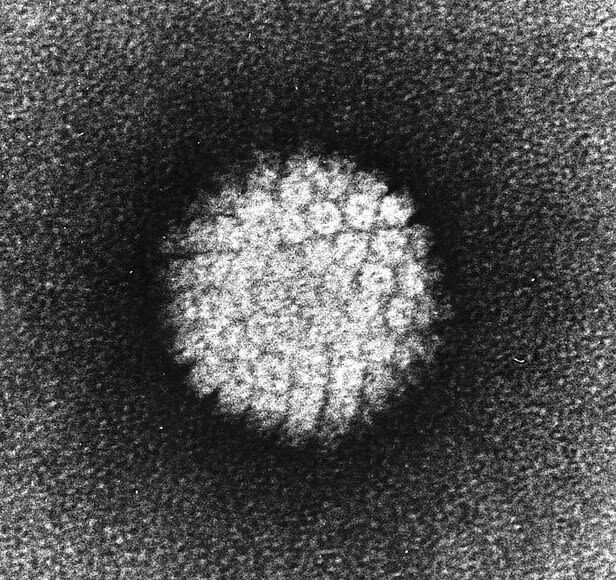
Electron micrograph of a negatively stained human papillomavirus (HPV) via Wikimedia Commons
Electron micrograph of a negatively stained human papillomavirus (HPV) via Wikimedia Commons

2002
Our researchers test a prototype HPV vaccine
Almost 10 years after the vaccine for HPV in cows had been developed, scientists developed the first human equivalent.
In an early-stage clinical trial, researchers in Manchester tested the prototype, and found that after three monthly doses, the healthy volunteers’ immune systems had made antibodies, proteins in our blood that fight infections, against HPV.



2003-2006
We show that testing for HPV infection before looking for cell changes could improve the screening programme by preventing even more cases of cervical cancer
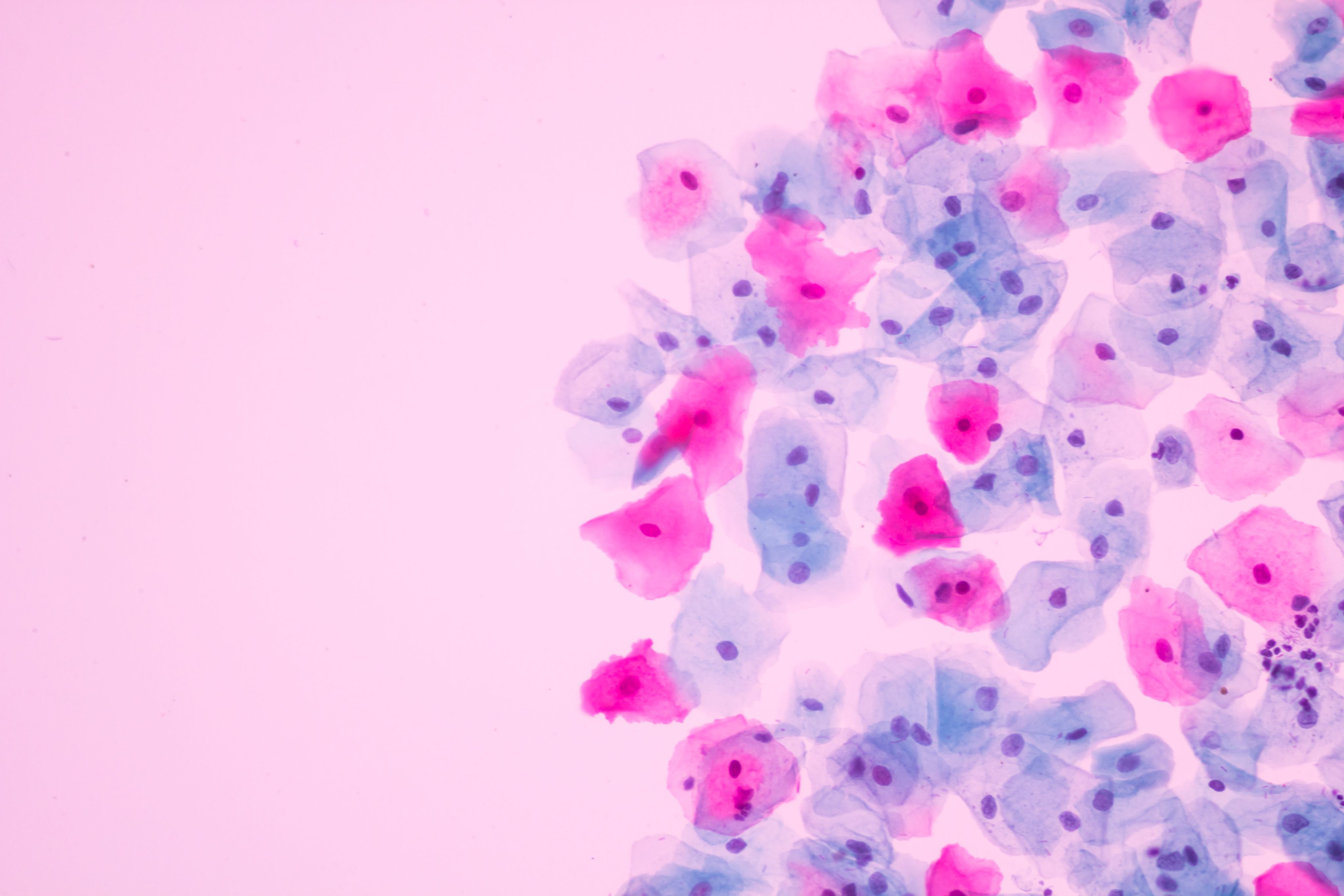
In two major studies, Professor Jack Cuzick and his team investigated how we could improve the cervical screening programme.
In the first, the HART study, they found that HPV testing could be done first in cervical screening instead of looking for abnormal cells. Women that tested positive for HPV were referred for cytology, where doctors would check their cervical cells for signs of abnormality.
If no abnormal cells were found, these women could be invited for another test 12 months later.
A few years later, they expanded their research to include data from over 60,000 women in Europe and North America. Their results showed that HPV testing was significantly more sensitive than cytology, meaning that fewer cases of the disease are missed.
Their results supported the use of HPV testing as the sole primary screening test, with cytology used only for women who test HPV positive.

A vial containing a dose of the HPV vaccine
A vial containing a dose of the HPV vaccine


2008
The HPV vaccination programme is rolled out to girls ages 11-13 in the UK
Between 2008 and 2014, over 2.3 million girls receive three doses of the HPV vaccine.

A teenage girl receiving a dose of the HPV vaccine. Shuttersock - Anola
A teenage girl receiving a dose of the HPV vaccine. Shuttersock - Anola


2017
Our research shows that people who’ve had the HPV vaccine could need fewer cervical screens
As the first cohorts of girls vaccinated against HPV began to reach the age where they would be invited for screening, researchers noted that the screening programme had not been adapted to take the vaccine into account.
Based on real data, they created a model that simulated various screening scenarios to determine whether the appropriate screening intensity differed between vaccinated and unvaccinated women.
They concluded that vaccinated women may be able to have just three cervical screens throughout their lifetime, compared to the current 12 offered – freeing up NHS resources while still protecting against cervical cancer. More research on how a woman’s vaccination status may be used in cervical screening is still ongoing.

2019
The HPV programme is offered to boys aged 11-13

A teenage boy receives a dose of the HPV vaccine. Shutterstock - Edson de Souza Nascimento
A teenage boy receives a dose of the HPV vaccine. Shutterstock - Edson de Souza Nascimento


2021
Our researchers prove the value of the HPV vaccine
The results of a monumental study we funded, led by Professor Peter Sasieni, found that the HPV vaccine was shown to dramatically reduce cervical cancer rates by almost 90% in women in their 20s who were offered it at ages 12 to 13.
“My immediate reaction was that we better check this – it’s too good to be true,” Sasieni said, when reflecting on the outcome of the study. “I thought that we might be reducing cases of cancer by 50%. And then to see over 80% reduction is just stunning.”
"In the UK, the elimination of cervical cancer as a public health problem in our lifetime is possible with continued action to improve access to vaccination and screening for all.”

2023
We show how changing the way we use existing drugs can cut the risk of cervical cancer returning
Since 1999, doctors have treated cervical cancer with a course of chemoradiation (CRT), a combination of chemotherapy and radiotherapy.
The INTERLACE trial investigated whether giving patients a six-week course of chemotherapy before CRT could reduce the risk of their disease returning.
Results from the trial show that after 5 years, the initial six weeks of chemotherapy cut the risk of their disease returning, or death, by 35%.
“This is the biggest improvement in outcome in this disease in over 20 years,” said Dr Mary McCormack, the lead investigator of the trial.

The road ahead
Over the last 70 years, our scientists have been pivotal in improving cervical screening and developing the HPV vaccine, preventing thousands of cancers every year. And they’ve improved treatment options for people with the disease.
But our work isn’t done yet.
We want to bring about a future where almost no-one develops cervical cancer. Where people in the UK and across the world can share in this progress equally, regardless of who they are or where they’re from.
References and further reading:
1958 - Wachtel, E. A suggestion for a cytological test of cancer cure. Ibid, 63: 176.











 Built with Shorthand
Built with Shorthand