The HPV vaccine
- HPV vaccination helps to prevent cancer by protecting against HPV. HPV increases the risk of some types of cancer and causes almost all cases of cervical cancer.
- The HPV vaccine is offered to all children between the ages of 11-13 in the UK.
- It is also available to people up to the age of 25 who missed their vaccination when offered it, men who have sex with men, and some transgender people.
The human papillomavirus (HPV) is a very common virus. It usually doesn’t cause any problems. For most people, HPV will be cleared from the body and they will never know they’ve had it.
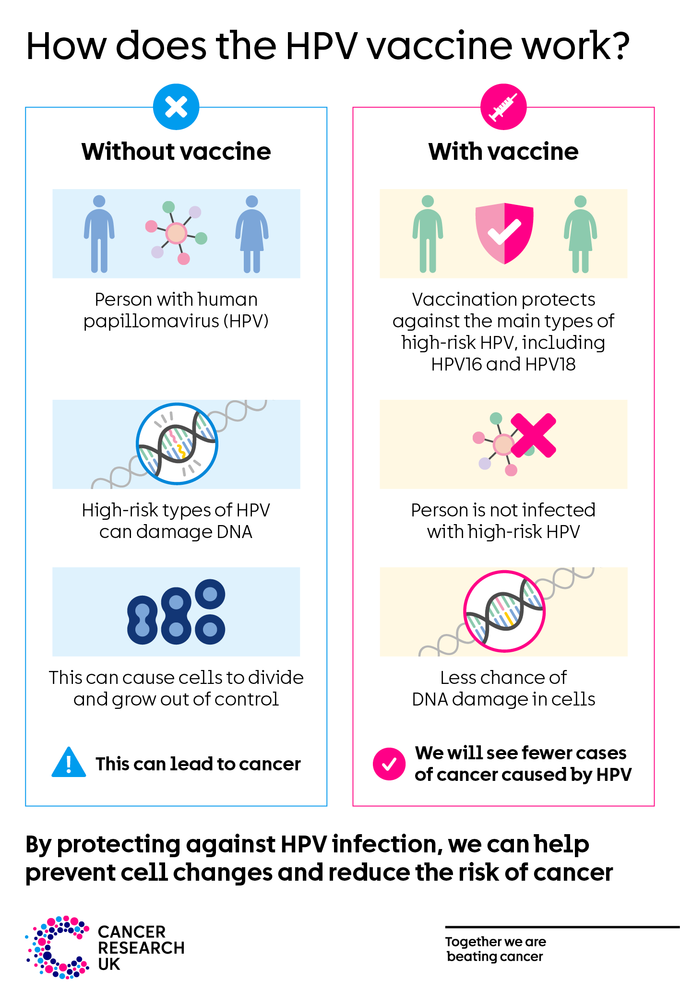
But some types of HPV can cause problems such as genital warts, and ‘high-risk’ types of HPV increase the risk of some cancers. High-risk HPV can cause changes to the DNA in our cells and make them more likely to turn cancerous.
Find out more about what HPV is and how it can cause cancer.
What is the HPV vaccine?
The HPV vaccine protects against HPV infection. The HPV vaccine used in the NHS vaccination programme is called Gardasil 9. It protects against nine types of HPV - HPV 6, 11, 16, 18, 31, 33, 45, 52 and 58.
Most people under the age of 25 will need just one dose of the vaccine.
Sometimes this vaccination is called the ‘cervical cancer vaccine’ because it has been proven to reduce rates of cervical cancer in England.
But the vaccine also protects against types of HPV that can cause cancers of the mouth, throat, vulva, vagina, penis and anus. It also protects against genital warts.
The NHS has further information on the HPV vaccine, including dosing and potential side effects.
Why get the HPV vaccine?
The HPV vaccine has been proven to be safe and effective at protecting against HPV and reducing HPV infections. This reduces the risk of cancers caused by HPV.
The HPV vaccine plays an important role in preventing cervical cancer, as almost all cases of cervical cancer are caused by HPV. HPV 16 and 18 cause about 7 in 10 cases of cervical cancer, and the vaccine protects against these HPV types.
As HPV is linked to cancers of the vulva, vagina, penis, anus and some types of mouth and throat cancer, the vaccine may also help lower the risk of these cancer types.
The vaccine also provides protection against genital warts, by protecting against HPV 6 and 11 which cause the majority of cases.
How does the HPV vaccine work?
The HPV vaccine tricks the body into thinking it has been exposed to the HPV virus. This triggers the body’s immune system to produce antibodies to fight against HPV. Antibodies are usually how our body clears an infection.
Because our immune system has a memory, the body will now be able to quickly recognise HPV and produce antibodies if the body is exposed to HPV in the future. This means it will be quicker and easier for the body to clear HPV.
Studies have already shown that protection by the HPV vaccine lasts for around 10 years. As the vaccine continues to be used, we expect studies will show that it lasts for much longer.
The NHS has more information on how vaccines work.
Who can get the HPV vaccine?
HPV vaccination is most effective in people who have not been exposed to HPV. This is why it’s recommended to vaccinate children at the age of 11-13. By adulthood most people will have been exposed to HPV, so vaccination won’t be as effective.
The groups listed below can get the HPV vaccine for free. If you aren’t in one of these groups, you can pay to have the vaccine privately if you want it.
Other people may be offered the vaccine for free on a case-by-case basis if they are at higher risk of HPV. If you’re not sure if you are eligible for the HPV vaccine or have questions about it, speak to your doctor.
All children aged 11-13
Since September 2019, all children aged 11-13 in the UK are offered the HPV vaccine. That’s all children in year 8 in England and Wales, year 9 in Northern Ireland, or S1 in Scotland. The vaccine is usually given in schools. Children who are home-schooled can get it via their GP.
People younger than 25 who missed their HPV vaccination
People who were offered the HPV vaccination but did not have it can still get the vaccine for free, up to the age of 25.
Talk to your GP, school nurse, or school immunisation team about this.
Men who have sex with men
Men who have sex with men can request the vaccine for free through sexual health and HIV clinics in the UK, up to the age of 45.
Studies show men who have sex with men may be at increased risk of anal cancer. Having the HPV vaccination may help to prevent anal cancer by protecting against HPV.
Transgender people
Some transgender (trans) people can get the vaccine for free through sexual health and HIV clinics in the UK:
- Trans men (men assigned female at birth) younger than 45 who have sex with other men
- Trans women (women assigned male at birth) younger than 45, on a case-by-case basis
But if you have already had the vaccine as part of the vaccination programme for school children, there is no need to have it again.
Do I need to go to cervical screening if I’ve had my HPV vaccination?
Yes, you should still consider taking part in cervical screening if you’ve had the HPV vaccine. The HPV vaccine doesn’t protect against all types of HPV that cause cervical cancer. And cervical screening is another effective way to prevent cervical cancer.
Cervical screening in the UK is for most women, some transgender men and some non-binary people who are aged between 25 and 64.
Cervical screening aims to detect HPV and spot early cell changes in the cervix caused by HPV. This means any abnormal cells can be monitored or treated before they have a chance to become cancer.
Cervical screening is for people without symptoms. Don’t wait for your next screening appointment if you’ve noticed anything that’s not normal for you, speak to your doctor.
Find out more about cervical screening
Find out more about cancer screening for people who are trans or non-binary
The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02178-4/fulltext
Lehtinen M, Lagheden C, Luostarinen T, et al. Ten-year follow-up of human papillomavirus vaccine efficacy against the most stringent cervical neoplasia end-point—registry-based follow-up of three cohorts from randomized trials. BMJ Open. 2017;7(8):e015867. doi:10.1136/bmjopen-2017-015867
National Health Service (NHS). HPV vaccine overview. NHS Website. 2019; (accessed March 2021). https://www.nhs.uk/conditions/vaccinations/hpv-human-papillomavirus-vaccine/
Last reviewed: 25 January 2024
Next review due: 25 January 2027