Dosing & Uses
Dosage Forms & Strengths
capsule
- 75mg
- 110mg
- 150mg
Stroke Prophylaxis With Atrial Fibrillation
Prevention of stroke and systemic embolism associated with nonvalvular atrial fibrillation
CrCl >30 mL/min: 150 mg PO BID
CrCl 15-30 mL/min: 75 mg PO BID
CrCl <15 mL/min or dialysis: No data available; not recommended
Dosage modifications (atrial fibrillation)
-
Renal impairment and coadministration with P-gp inhibitors
- CrCl 30-50 mL/min and coadministration with dronedarone or systemic ketoconazole: Reduce dose to 75 mg BID (dose adjustment is not necessary when coadministered with other P-gp inhibitors)
- CrCl <30 mL/min with concomitant use of any P-gp inhibitor: Avoid coadministration
AHA/ACC/HRS guidelines for atrial fibrillation
- Class 1: For patients with AF or atrial flutter <48-hour duration and with high risk of stroke, IV heparin or LMWH, or administration of a factor Xa or direct thrombin inhibitor, is recommended as soon as possible before or immediately after cardioversion, followed by long-term anticoagulation therapy
- Class IIa: For patients with AF or atrial flutter of ≥48-hr, or when the duration of AF is unknown, anticoagulation with warfarin (INR 2-3), a factor Xa inhibitor, or direct thrombin inhibitor is recommended for at least 3 weeks prior to and 4 weeks after cardioversion
- Class IIb: For patients with AF or atrial flutter <48-hour duration who are at low thromboembolic risk, anticoagulation (IV heparin, LMWH, or a new oral anticoagulant) or no antithrombotic therapy may be considered for cardioversion, without the need for postcardioversion oral anticoagulation
- For patients with nonvalvular AF unable to maintain a therapeutic INR level with warfarin, use of a direct thrombin or factor Xa inhibitor
- Not recommended in patients with AF and end-stage CKD or on hemodialysis because of the lack of evidence from clinical trials regarding the balance of risks and benefits; warfarin or apixaban recommended
- Circulation July 9, 2019
DVT or PE Treatment
Indicated for treatment of deep vein thrombosis (DVT) and pulmonary embolus (PE) in patients who have been treated with a parenteral anticoagulant for 5-10 days
Also indicated to reduce the risk of recurrence of DVT and PE in patients who have been previously treated
CrCl >30 mL/min: 150 mg PO BID
CrCl ≤30 mL/min or on dialysis: Dosage recommendations cannot be provided
CrCl <50 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration
DVT or PE Prophylaxis
Indicated for the prophylaxis of DVT and PE following hip replacement surgery
CrCl >30 mL/min: 110 mg PO 1-4 hr after surgery and after hemostasis has been achieved on first day, then 220 mg taken qDay for 28-35 days
If dabigatran is not started on the day of surgery, after hemostasis has been achieved initiate treatment with 220 mg qDay
CrCl ≤30 mL/min or on dialysis: Dosing recommendations cannot be provided
CrCl <50 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration
Dosing Considerations
Different dosage forms
- Available in different dosage forms (ie, capsules for adults or children aged 8 to <18 years, oral pellets for children aged 3 months to <12 years) and not all dosage forms are approved for the same indications and age groups
- Additionally, there are differences between dosage forms with respect to dosing owing different bioavailability
- Do not substitute different dosage forms (for example, capsules) for oral pellets on a milligram-to-milligram basis and do not combine more than 1 dosage form to achieve the total dose
Converting to dabigatran from warfarin or parenteral anticoagulants
- Converting from warfarin: Discontinue warfarin and initiate dabigatran when INR <2.0
- Converting from parenteral anticoagulant: Give dabigatran 0-2 hours before time for next dose of the parenteral drug that was to have been administered or initiate at time of discontinuing continuous IV heparin
Converting from dabigatran to warfarin or parenteral anticoagulants
- CrCl ≥50 mL/min: Start warfarin 3 days before discontinuing dabigatran
- CrCl 30-50 mL/min: Start warfarin 2 days before discontinuing dabigatran
- CrCl 15-30 mL/min: Start warfarin 1 day before discontinuing dabigatran
- CrCl <15 mL/min: No recommendations can be made
- Converting to parenteral anticoagulant: Wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after last dabigatran dose before initiating parenteral anticoagulant
Discontinuation for surgery and other interventions
- If possible, discontinue dabigatran 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding
- Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required
- If surgery cannot be delayed, there is increased risk of bleeding; this risk of bleeding should be weighed against urgency of intervention; use a specific reversal agent (idarucizumab) in case of emergency surgery or urgent procedures when reversal of anticoagulant effect of dabigatran is needed; refer to idarucizumab prescribing information for additional information
- Restart dabigatran capsules as soon as medically appropriate
Dosage Forms & Strengths
capsule
- 75mg
- 110mg
- 150mg
oral pellets
- 20mg
- 30mg
- 40mg
- 50mg
- 110mg
- 150mg
VTE Treatment or Prevention
Indicated for treatment of venous thromboembolic events (VTE) in pediatric patients aged >3 months to <18 years who have been treated with a parenteral anticoagulant for at least 5 days
Also indicated to reduce risk of recurrent VTEs in pediatric patients aged 3 months to <18 years who have been previously treated
<3 months: Safety and efficacy not established
3 months to <2 years (oral pellets)
- Adjust dose according to age and actual weight as treatment progresses
- 3 to <4 kg (3 to <6 months): 30 mg PO BID
- 4 to <5 kg (3 to <10 months): 40 mg PO BID
- 5 to <7 kg (3 to <5 months): 40 mg PO BID
- 5 to <7 kg (5 to <24 months): 50 mg PO BID
- 7 kg to <9 kg (3 to <4 months): 50 mg PO BID
- 7 kg to <9 kg (4 to <9 months): 60 mg PO BID
- 7 kg to <9 kg (9 to <24 months): 70 mg PO BID
- 9 kg to <11 kg (5 to <6 months): 60 mg PO BID
- 9 kg to <11 kg (6 to <11 months): 80 mg PO BID
- 9 kg to <11 kg (11 to <24 months): 90 mg PO BID
- 11 to <13 kg (8 to <18 months): 100 mg PO BID
- 11 to <13 kg (18 to <24 months): 110 mg PO BID
- 13 to <16 kg (10 to <11 months): 100 mg PO BID
- 13 to <16 kg (11 to <24 months): 140 mg PO BID
- 16 kg to <21 kg (12 to <24 months): 140 mg PO BID
- 21 kg to <26 kg (18 to <24 months): 180 mg PO BID
2 to <12 years (oral pellets)
- 7 to <9 kg: 70 mg PO BID
- 9 to <11 kg: 90 mg PO BID
- 11 to <13 kg: 110 mg PO BID
- 13 to <16 kg: 140 mg PO BID
- 16 to <21 kg: 170 mg PO BID
- 21 to <41 kg: 220 mg PO BID
- >41 kg: 260 mg PO BID
8 to <18 years (capsules)
- May use for older children or adolescents who can swallow the capsule whole
- Dosage based on actual weight
- 11 to <16 kg: 75 mg PO BID
- 16 to <26 kg: 110 mg PO BID
- 26 to <41 kg: 150 mg PO BID
- 41 to <61 kg: 185 mg PO BID
- 61 to <81 kg: 220 mg PO BID
- >81 kg: 260 mg PO BID
Dosage Modifications
Renal impairment (pellets or capsules)
- eGFR >50 mL/min/1.73 m2: No dosage adjustment required
- eGFR <50 mL/min/1.73 m2: Avoid use owing to lack of pediatric data
Dosing Considerations
Different dosage forms
- Available in different dosage forms (ie, capsules for adults or children aged 8 to <18 years, oral pellets for children aged 3 months to <12 years) and not all dosage forms are approved for the same indications and age groups
- Additionally, there are differences between dosage forms with respect to dosing owing different bioavailability
- Do not substitute different dosage forms (for example, capsules) for oral pellets on a milligram-to-milligram basis and do not combine more than 1 dosage form to achieve the total dose
Converting to dabigatran from warfarin or parenteral anticoagulants
- Converting from warfarin: Discontinue warfarin and initiate dabigatran when INR <2.0
- Converting from parenteral anticoagulant: Give dabigatran 0-2 hours before time for next dose of the parenteral drug that was to have been administered or initiate at time of discontinuing continuous IV heparin
Converting from dabigatran to warfarin or parenteral anticoagulants
- eGFR ≥50 mL/min/1.73 m2: Start warfarin 3 days before discontinuing dabigatran capsules
- eGFR <50 mL/min/1.73 m2: Not studied; avoid dabigatran capsules/pellets in these patients
- Wait 12 hr after last dose of oral pellets or capsule before switching to parenteral anticoagulant
Discontinuation for surgery and other interventions
- Discontinue dabigatran pellets/capsules 24 hr before an elective surgery (eGFR >80 mL/min/1.73 m2) or 2 days before an elective surgery (eGFR 50-80 mL/min/1.73 m2)
- Pediatric patients with an eGFR <50 mL/min/1.73 m2 have not been studied; avoid use of dabigatran pellets/ capsules in these patients
Increases risk of bleeding; bleeding can be significant and sometimes fatal; risk for bleeding or stroke increases with age >75 years
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (3)
- defibrotide
defibrotide increases effects of dabigatran by pharmacodynamic synergism. Contraindicated. Coadministration of defibrotide is contraindicated with antithrombotic/fibrinolytic drugs. This does not include use for routine maintenance or reopening of central venous lines.
- mifepristone
mifepristone, dabigatran. Other (see comment). Contraindicated. Comment: Mifepristone may lead to excessive post abortion bleeding in pts. on anticoagulant therapy.
- prothrombin complex concentrate, human
dabigatran, prothrombin complex concentrate, human. pharmacodynamic synergism. Contraindicated.
Serious - Use Alternative (32)
- antithrombin alfa
antithrombin alfa and dabigatran both increase anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- antithrombin III
antithrombin III and dabigatran both increase anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- apixaban
dabigatran and apixaban both increase anticoagulation. Avoid or Use Alternate Drug.
- caplacizumab
caplacizumab, dabigatran. Either increases effects of the other by anticoagulation. Avoid or Use Alternate Drug.
- carbamazepine
carbamazepine decreases levels of dabigatran by increasing metabolism. Avoid or Use Alternate Drug. The concomitant use of dabigatran and P-gp inducers should generally be avoided.
carbamazepine will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran - dalteparin
dabigatran and dalteparin both increase anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- doxorubicin liposomal
doxorubicin liposomal will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- dronedarone
dronedarone will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Atrial fibrillation: Decrease dabigatran dose when coadministered with dronedarone if CrCl is 30-50 mL/min. Avoid coadministering dabigatran with dronedarone if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with dronedarone if CrCl <50 mL/min
- edoxaban
edoxaban, dabigatran. Either increases toxicity of the other by anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding, monitor closely. Promptly evaluate any signs or symptoms of blood loss. Long-term concomitant treatment with edoxaban and other anticoagulants is not recommended. Short-term coadministration may be needed for patients transitioning to or from edoxaban.
- enoxaparin
dabigatran and enoxaparin both increase anticoagulation. Avoid or Use Alternate Drug. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- erdafitinib
erdafitinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If coadministration unavoidable, separate administration by at least 6 hr before or after administration of P-gp substrates with narrow therapeutic index.
- fondaparinux
dabigatran and fondaparinux both increase anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- fosphenytoin
fosphenytoin will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- heparin
dabigatran and heparin both increase anticoagulation. Avoid or Use Alternate Drug. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- ivacaftor
ivacaftor increases levels of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min.
- ketoconazole
ketoconazole will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Atrial fibrillation: Decrease dabigatran dose when coadministered with ketoconazole if CrCl is 30-50 mL/min. Avoid coadministering dabigatran with ketoconazole if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with ketoconazole if CrCl <50 mL/min
- lasmiditan
lasmiditan increases levels of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
- levoketoconazole
levoketoconazole will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Atrial fibrillation: Decrease dabigatran dose when coadministered with ketoconazole if CrCl is 30-50 mL/min. Avoid coadministering dabigatran with ketoconazole if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with ketoconazole if CrCl <50 mL/min
- nefazodone
nefazodone will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug.
- phenobarbital
phenobarbital will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- phenytoin
phenytoin will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- primidone
primidone will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- rifampin
rifampin will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- sotorasib
sotorasib will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If use is unavoidable, refer to the prescribing information of the P-gp substrate for dosage modifications.
- St John's Wort
St John's Wort will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- tenofovir DF
tenofovir DF will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- tepotinib
tepotinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. If concomitant use unavoidable, reduce the P-gp substrate dosage if recommended in its approved product labeling.
- tipranavir
tipranavir increases effects of dabigatran by pharmacodynamic synergism. Avoid or Use Alternate Drug. Tipranavir has mild antiplatelet activity that may incr bleeding risk. The concomitant use of dabigatran and P-gp inducers should generally be avoided. .
tipranavir will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran - vinblastine
vinblastine will decrease the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Avoid or Use Alternate Drug. Avoid coadministration. P-gp inducers reduce systemic exposure of dabigatran
- vortioxetine
vortioxetine and dabigatran both increase anticoagulation. Avoid or Use Alternate Drug.
- warfarin
dabigatran increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- zanubrutinib
dabigatran, zanubrutinib. Either increases effects of the other by anticoagulation. Avoid or Use Alternate Drug.
Monitor Closely (162)
- abciximab
dabigatran, abciximab. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- abiraterone
abiraterone will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- acalabrutinib
acalabrutinib increases effects of dabigatran by anticoagulation. Use Caution/Monitor. Coadministration of acalabrutinib with antiplatelets or anticoagulants may further increase risk of hemorrhage. Monitor for signs of bleeding and consider the benefit-risk of withholding acalabrutinib for 3-7 days presurgery and postsurgery depending upon the type of surgery and the risk of bleeding.
- afatinib
afatinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- agrimony
dabigatran and agrimony both increase anticoagulation. Modify Therapy/Monitor Closely.
- alfalfa
dabigatran and alfalfa both increase anticoagulation. Modify Therapy/Monitor Closely.
- alteplase
dabigatran and alteplase both increase anticoagulation. Modify Therapy/Monitor Closely. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- American ginseng
dabigatran and American ginseng both increase anticoagulation. Modify Therapy/Monitor Closely.
- amiodarone
amiodarone will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- anagrelide
dabigatran, anagrelide. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- anamu
dabigatran and anamu both increase anticoagulation. Use Caution/Monitor.
- argatroban
argatroban and dabigatran both increase anticoagulation. Modify Therapy/Monitor Closely. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- aspirin
dabigatran and aspirin both increase anticoagulation. Modify Therapy/Monitor Closely. Both drugs have the potential to cause bleeding. The need for simultaneous use of low-dose aspirin (<100 mg/day) with anticoagulants are common for patients with cardiovascular disease, but may result in increased bleeding; monitor closely. Promptly evaluate any signs or symptoms of blood loss if treated concomitantly with low-dose aspirin. Avoid coadministration with chronic use of higher dose aspirin
- aspirin rectal
dabigatran and aspirin rectal both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- aspirin/citric acid/sodium bicarbonate
dabigatran and aspirin/citric acid/sodium bicarbonate both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- atorvastatin
atorvastatin will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- azficel-T
azficel-T, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Coadministration with anticoagulants or antiplatelets may increase bruising or bleeding at biopsy and/or injection sites; concomitant use not recommended. Decisions regarding continued use or cessation of anticoagulants or antiplatelets should be made by a physician.
- azithromycin
azithromycin will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- berotralstat
berotralstat will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor or titrate P-gp substrate dose if coadministered.
- betrixaban
dabigatran, betrixaban. Either increases levels of the other by anticoagulation. Use Caution/Monitor.
- bivalirudin
bivalirudin and dabigatran both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- carvedilol
carvedilol will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- celecoxib
dabigatran and celecoxib both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- chitosan
chitosan increases effects of dabigatran by Other (see comment). Use Caution/Monitor. Comment: Chitosan can decrease GI absorption of vitamin K, enhancing anticoagulant effects.
- choline magnesium trisalicylate
dabigatran and choline magnesium trisalicylate both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- cilostazol
dabigatran, cilostazol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- cinnamon
dabigatran and cinnamon both increase anticoagulation. Modify Therapy/Monitor Closely.
- citalopram
citalopram increases effects of dabigatran by pharmacodynamic synergism. Use Caution/Monitor. Combination may increase risk of bleeding.
- clarithromycin
clarithromycin will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- clopidogrel
dabigatran, clopidogrel. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- cobicistat
cobicistat will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- collagenase clostridium histolyticum
dabigatran increases toxicity of collagenase clostridium histolyticum by anticoagulation. Use Caution/Monitor. Collagenase clostridium histolyticum has high incidence of ecchymosis/contusion at injection site; avoid concomitant anticoagulants (except for low-dose aspirin, ie, up to 150 mg/day).
- cordyceps
dabigatran and cordyceps both increase anticoagulation. Modify Therapy/Monitor Closely.
- cornsilk
cornsilk decreases effects of dabigatran by pharmacodynamic antagonism. Use Caution/Monitor. Cornsilk contains vitamin K; consume a consistent amount daily.
- crizotinib
crizotinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- cyclosporine
cyclosporine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- danicopan
danicopan will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Danicopan increases plasma concentrations of P-gp substrates; consider dose reduction of P-gp substrates where minimal concentration changes may lead to serious adverse reactions.
- danshen
dabigatran and danshen both increase anticoagulation. Use Caution/Monitor.
- darunavir
darunavir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. P-gp inhibitors may increase systemic exposure of dabigatran in patients with renal impairment.
- deferasirox
deferasirox, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Gastric ulceration and GI bleeding have been reported in patients taking deferasirox, use caution when coadministering with other drugs known to increase the risk of peptic ulcers or gastric hemorrhage including anticoagulants.
- desirudin
dabigatran and desirudin both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- devil's claw
dabigatran and devil's claw both increase anticoagulation. Use Caution/Monitor.
- diclofenac
dabigatran and diclofenac both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- diflunisal
dabigatran and diflunisal both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
diflunisal increases effects of dabigatran by plasma protein binding competition. Use Caution/Monitor. - dipyridamole
dabigatran, dipyridamole. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
dipyridamole will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min - divalproex sodium
divalproex sodium will decrease the level or effect of dabigatran by unknown mechanism. Use Caution/Monitor.
- dong quai
dabigatran and dong quai both increase anticoagulation. Modify Therapy/Monitor Closely.
- elagolix
elagolix will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
- eliglustat
eliglustat will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- elvitegravir/cobicistat/emtricitabine/tenofovir DF
elvitegravir/cobicistat/emtricitabine/tenofovir DF will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- epoprostenol
dabigatran and epoprostenol both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- eptifibatide
dabigatran, eptifibatide. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- erythromycin base
erythromycin base will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- erythromycin ethylsuccinate
erythromycin ethylsuccinate will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- erythromycin lactobionate
erythromycin lactobionate will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- erythromycin stearate
erythromycin stearate will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- ethanol
ethanol increases effects of dabigatran by unknown mechanism. Use Caution/Monitor. Acute EtOH intoxication.
- ethotoin
dabigatran increases levels of ethotoin by unknown mechanism. Use Caution/Monitor.
ethotoin, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Hydantoin anticonvulsants increase anticoagulant effects at first, then decrease those effects with continued use (2+ wks). There are multiple mechanisms involved, including enzyme induction, plasma protein binding site competition, and additive effects on prothrombin time. - etodolac
dabigatran and etodolac both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- etravirine
etravirine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- fennel
dabigatran and fennel both increase anticoagulation. Modify Therapy/Monitor Closely.
- fenoprofen
dabigatran and fenoprofen both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- feverfew
dabigatran and feverfew both increase anticoagulation. Modify Therapy/Monitor Closely.
- fish oil
fish oil, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Patients taking fish oil and an anticoagulant or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding. .
- fish oil triglycerides
fish oil triglycerides will increase the level or effect of dabigatran by anticoagulation. Use Caution/Monitor. Prolonged bleeding reported in patients taking antiplatelet agents or anticoagulants and oral omega-3 fatty acids. Periodically monitor bleeding time in patients receiving fish oil triglycerides and concomitant antiplatelet agents or anticoagulants.
- fluorouracil
fluorouracil increases effects of dabigatran by unspecified interaction mechanism. Use Caution/Monitor. Due to the thrombocytopenic effects of fluorouracil additive risk of bleeding may be seen in patients receiving concomitant anticoagulants.
- flurbiprofen
dabigatran and flurbiprofen both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- forskolin
dabigatran and forskolin both increase anticoagulation. Modify Therapy/Monitor Closely.
- fostamatinib
fostamatinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Concomitant use of fostamatinib may increase concentrations of P-gp substrates. Monitor for toxicities of the P-gp substrate drug that may require dosage reduction when given concurrently with fostamatinib.
- garlic
dabigatran and garlic both increase anticoagulation. Modify Therapy/Monitor Closely.
- ginger
dabigatran and ginger both increase anticoagulation. Modify Therapy/Monitor Closely.
- ginkgo biloba
dabigatran and ginkgo biloba both increase anticoagulation. Modify Therapy/Monitor Closely.
- glecaprevir/pibrentasvir
glecaprevir/pibrentasvir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor.
- grapefruit
grapefruit will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- green tea
green tea, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Combination may increase risk of bleeding, caution is advised.
- hemin
dabigatran, hemin. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Hemin degradation product (ie, hematin) may produce coagulopathy (eg, thrombocytopenia, platelet degranulation) and cause mild anticoagulant effects.
- horse chestnut seed
dabigatran and horse chestnut seed both increase anticoagulation. Modify Therapy/Monitor Closely.
- ibrutinib
ibrutinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
ibrutinib, dabigatran. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Ibrutinib may potentiate the effects of anticoagulant agents such as warfarin may increase the risk of bleeding; monitor for signs of bleeding.
dabigatran, ibrutinib. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Ibrutinib may potentiate the effects of anticoagulant agents such as warfarin may increase the risk of bleeding; monitor for signs of bleeding. - ibuprofen
dabigatran and ibuprofen both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- ibuprofen IV
dabigatran and ibuprofen IV both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- icosapent
icosapent, dabigatran. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Icosapent may prolong bleeding time; monitor periodically if coadministered with other drugs that affect bleeding.
- iloprost inhaled
dabigatran and iloprost inhaled both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- imatinib
imatinib, dabigatran. Either increases toxicity of the other by Other (see comment). Modify Therapy/Monitor Closely. Comment: Imatinib may cause thrombocytopenia; bleeding risk increased when imatinib is coadministered with anticoagulants, NSAIDs, platelet inhibitors, and thrombolytic agents; patients requiring anticoagulation while on imatinib should receive LMWH or unfractionated heparin instead of warfarin because of multiple interaction mechanisms of imatinib with warfarin.
- indomethacin
dabigatran and indomethacin both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- istradefylline
istradefylline will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Istradefylline 40 mg/day increased peak levels and AUC of P-gp substrates in clinical trials. Consider dose reduction of sensitive P-gp substrates.
- itraconazole
itraconazole will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- ketoprofen
dabigatran and ketoprofen both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- ketorolac
dabigatran and ketorolac both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- ketorolac intranasal
dabigatran and ketorolac intranasal both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- lapatinib
lapatinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- ledipasvir/sofosbuvir
ledipasvir/sofosbuvir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- lenacapavir
lenacapavir will increase the level or effect of dabigatran by Other (see comment). Use Caution/Monitor. Refer to the prescribing information for concomitant administration with combined moderate CYP3A inhibitors.
- levetiracetam
levetiracetam will decrease the level or effect of dabigatran by unknown mechanism. Use Caution/Monitor.
- lomitapide
lomitapide will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- lonafarnib
lonafarnib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Lonafarnib is a weak P-gp inhibitor. Monitor for adverse reactions if coadministered with P-gp substrates where minimal concentration changes may lead to serious or life-threatening toxicities. Reduce P-gp substrate dose if needed.
- lopinavir
lopinavir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- meclofenamate
dabigatran and meclofenamate both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- mefenamic acid
dabigatran and mefenamic acid both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- mefloquine
mefloquine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- melatonin
melatonin increases effects of dabigatran by anticoagulation. Use Caution/Monitor. Melatonin may decrease prothrombin time.
- meloxicam
dabigatran and meloxicam both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- mistletoe
dabigatran increases and mistletoe decreases anticoagulation. Effect of interaction is not clear, use caution. Modify Therapy/Monitor Closely.
- nabumetone
dabigatran and nabumetone both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- naproxen
dabigatran and naproxen both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- nelfinavir
nelfinavir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- neratinib
neratinib increases levels of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Neratinib inhibits P-gp transport. Caution if coadministered with a P-gp substrate with a narrow therapeutic index.
- nettle
dabigatran increases and nettle decreases anticoagulation. Effect of interaction is not clear, use caution. Modify Therapy/Monitor Closely.
- nicardipine
nicardipine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- nifedipine
nifedipine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- nilotinib
nilotinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- nintedanib
nintedanib increases effects of dabigatran by anticoagulation. Use Caution/Monitor. Nintedanib is a VEGFR inhibitor, and may increase the risk of bleeding; monitor patients on full anticoagulation therapy; monitor closely for bleeding and adjust therapy as needed .
- nirmatrelvir/ritonavir
nirmatrelvir/ritonavir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Clinical significance dependent on degree of renal impairment. Dabigatran is mainly cleared by glomerular filtration. The prodrug of dabigatran is a substrate of P-gp and concentrations may increase due to inhibition of P-gp by ritonavir. Dabigatran dose may need to be reduced in patients with mild/moderate renal impairment if coadministered with a P-gp inhibitor. Dabigatran is not recommended in patients with severe renal impairment.
- omega 3 carboxylic acids
omega 3 carboxylic acids, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Patients taking omega-3 acids and an anticoagulant or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding.
- omega 3 fatty acids
omega 3 fatty acids, dabigatran. Other (see comment). Use Caution/Monitor. Comment: Patients taking omega-3-fatty acids and an anticoagulant or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding. .
- oxaprozin
dabigatran and oxaprozin both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- paliperidone
paliperidone will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- panax ginseng
dabigatran and panax ginseng both increase anticoagulation. Modify Therapy/Monitor Closely.
- pau d'arco
dabigatran and pau d'arco both increase anticoagulation. Modify Therapy/Monitor Closely.
- pegaspargase
pegaspargase increases effects of dabigatran by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of bleeding events.
- pentosan polysulfate sodium
dabigatran and pentosan polysulfate sodium both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- piroxicam
dabigatran and piroxicam both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- ponatinib
ponatinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- porfimer
dabigatran decreases effects of porfimer by pharmacodynamic antagonism. Use Caution/Monitor.
- posaconazole
posaconazole will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- prasugrel
dabigatran, prasugrel. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- pretomanid
pretomanid will increase the level or effect of dabigatran by Other (see comment). Use Caution/Monitor. Increase monitoring for drug-related adverse effects if pretomanid is coadministered with sensitive P-gp substrates.
- progesterone micronized
progesterone micronized will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- propafenone
propafenone will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- propranolol
propranolol will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- quinidine
quinidine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- quinine
quinine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- ranolazine
ranolazine will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- reishi
dabigatran and reishi both increase anticoagulation. Modify Therapy/Monitor Closely.
- reteplase
dabigatran and reteplase both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- rifabutin
rifabutin decreases levels of dabigatran by increasing metabolism. Use Caution/Monitor. The concomitant use of dabigatran and P-gp inducers should generally be avoided.
- ritonavir
ritonavir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- rivaroxaban
rivaroxaban, dabigatran. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Avoid concurrent use of rivaroxaban with other anticoagulants due to increased bleeding risk other than during therapeutic transition periods where patients should be observed closely. Monitor for signs/symptoms of blood loss.
- salsalate
dabigatran and salsalate both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- saquinavir
saquinavir will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- sarecycline
sarecycline will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Monitor for toxicities of P-gp substrates that may require dosage reduction when coadministered with P-gp inhibitors.
- saw palmetto
saw palmetto increases toxicity of dabigatran by unspecified interaction mechanism. Use Caution/Monitor. May increase risk of bleeding.
- Siberian ginseng
dabigatran and Siberian ginseng both increase anticoagulation. Modify Therapy/Monitor Closely.
- sodium zirconium cyclosilicate
sodium zirconium cyclosilicate will decrease the level or effect of dabigatran by increasing gastric pH. Applies only to oral form of both agents. Modify Therapy/Monitor Closely. Separate administration by at least 2 hr.
- stiripentol
stiripentol will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Modify Therapy/Monitor Closely. Consider reducing the dose of P-glycoprotein (P-gp) substrates, if adverse reactions are experienced when administered concomitantly with stiripentol.
- sulindac
dabigatran and sulindac both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- sunitinib
sunitinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- suvorexant
suvorexant will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- tacrolimus
tacrolimus will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- tamoxifen
tamoxifen will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- tenecteplase
dabigatran and tenecteplase both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- ticagrelor
ticagrelor, dabigatran. Either increases effects of the other by anticoagulation. Use Caution/Monitor. According to official packaging labeling, dose adjustment of oral dabigatran not required when coadministered with oral dose of ticagrelor.
ticagrelor will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min - ticlopidine
dabigatran, ticlopidine. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- tirofiban
dabigatran, tirofiban. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- tolmetin
dabigatran and tolmetin both increase anticoagulation. Use Caution/Monitor. Caution is advised, both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- treprostinil
dabigatran and treprostinil both increase anticoagulation. Use Caution/Monitor. Both drugs have the potential to cause bleeding. Concomitant use may increase risk of bleeding.
- tucatinib
tucatinib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Consider reducing the dosage of P-gp substrates, where minimal concentration changes may lead to serious or life-threatening toxicities.
- ulipristal
ulipristal will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- valproic acid
valproic acid will decrease the level or effect of dabigatran by unknown mechanism. Use Caution/Monitor.
- vandetanib
vandetanib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- vemurafenib
vemurafenib will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- verapamil
verapamil will increase the level or effect of dabigatran by P-glycoprotein (MDR1) efflux transporter. Use Caution/Monitor. Atrial fibrillation: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <30 mL/min. DVT/PE treatment: Avoid coadministering dabigatran with P-gp inhibitors if CrCl <50 mL/min
- vorapaxar
dabigatran, vorapaxar. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Coadministration of anticoagulants, antiplatelets, or other drug affecting coagulation should be monitored periodically due to potential increased risk of bleeding.
Minor (3)
- chlorella
chlorella decreases effects of dabigatran by pharmacodynamic antagonism. Minor/Significance Unknown. Theoretical, due to vitamin K content.
- mineral oil
mineral oil decreases levels of dabigatran by inhibition of GI absorption. Applies only to oral form of both agents. Minor/Significance Unknown.
- verteporfin
dabigatran decreases effects of verteporfin by pharmacodynamic antagonism. Minor/Significance Unknown.
Adverse Effects
>10%
Adults
- Dyspepsia and gastritis (35%; compared with warfarin [24%])
- Any bleed (16.6%; compared with warfarin [18.4%])
Pediatrics
- GI adverse effects (32%; compared with standard of care [SOC] with warfarin, LMWH, or fondaparinux [12%])
- Any bleeding (22%; SOC 24%)
- Minor bleeding (19%; SOC 23%)
1-10%
Adults
- Major bleed (3.47%/y; compared with warfarin [3.58%/y])
- GI bleed (1.59%/y; compared with warfarin [1.51%/y])
Pediatrics
- Major and clinically relevant nonmajor bleeding (3.4%; SOC 3.3%)
- Major bleeding (2.3%; SOC 2.2%)
- Clinically relevant nonmajor bleeding (1.1%; SOC 1.1%)
<1%
Adults
- Intracranial hemorrhage (0.22%/y; compared with warfarin [0.77%/y])
- Hypersensitivity, including urticaria, rash, pruritus (<0.1%)
Postmarketing Reports
Adults
- Angioedema
- Neutropenia
- Agranulocytosis
- Esophageal ulcers
- Thrombocytopenia
- Alopecia
- Vomiting
- Nausea
- Diarrhea
- Anticoagulant-related nephropathy
Warnings
Black Box Warnings
Premature discontinuation
- Premature discontinuation of any oral anticoagulant, including dabigatran, increases the risk of thrombotic events
- If dabigatran must be discontinued for a reason other than pathological bleeding, consider coverage with another anticoagulant
Spinal/epidural hematoma
- Epidural or spinal hematomas may occur in patients who are receiving neuraxial anesthesia or undergoing spinal puncture
- These hematomas may result in long-term or permanent paralysis
- Monitor patients frequently for signs and symptoms of neurological impairment; if neurological compromise is noted, urgent treatment is necessary
- Consider the benefits and risks before neuraxial intervention in patients who are anticoagulated or to be anticoagulated
-
Factors that can increase risk include:
- Indwelling epidural catheters
- Coadministration with other drugs that affect hemostasis (eg, NSAIDs, platelet inhibitors, other anticoagulants)
- History of traumatic or repeated epidural or spinal punctures
- History of spinal deformity or spinal surgery
- Optimal timing is unknown between dabigatran administration and neuraxial procedures
Contraindications
Hypersensitivity to drug or excipients
Active pathologic bleeding
Mechanical prosthetic heart valves
- Significantly more thromboembolic events (eg, valve thrombosis, stroke, TIAs, MI) observed with dabigatran than with warfarin
- Excessive major bleeding (predominantly postoperative pericardial effusions requiring intervention for hemodynamic compromise) observed with dabigatran, compared with warfarin
- These bleeding and thromboembolic events, seen in the RE-ALIGN study (Am Heart J, June 2012), were observed in patients who were started on dabigatran postoperatively within 3 days after mechanical bileaflet valve implantation, as well as in patients whose valves had been implanted more than 3 months prior to enrollment in the study; this clinical trial was terminated early because of these events
Cautions
Premature discontinuation of oral anticoagulants (other than pathological bleeding) in the absence of adequate alternative anticoagulation increases risk of thrombotic events
Direct-acting oral anticoagulants (DOACs) not recommended for use in patients with triple-positive antiphospholipid syndrome (APS); for patients with APS (especially those who are triple-positive [positive for lupus anticoagulant, anticardiolipin, and anti-beta 2-glycoprotein I antibodies]), treatment with DOACs has been associated with increased rates of recurrent thrombotic events compared with vitamin K antagonist therapy
Spinal/epidural anesthesia or puncture
- When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis
- Consider dabigatran pharmacokinetic profile; placement or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect is low; however, the exact timing to reach a sufficiently low anticoagulant effect in each patient is not known
Coadministration with P-gp inducers and inhibitors
- P-gp inducers (eg, rifampin) reduce exposure to dabigatran and should generally be avoided
- P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran
- Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone
- Concomitant use of dabigatran capsules with P-gp-inhibitors has not been studied in pediatric patients but may increase exposure to dabigatran
- DVT/PE treatment/prevention, renal impairment, and P-gp inhibitors: Avoid coadministration if CrCl <50 mL/min
- VTE in pediatric patients: Not studied, but P-gp inhibitors may increase dabigatran exposure
-
AF treatment, renal impairment, and P-gp inhibitors
- CrCl 30-50 mL/min and P-gp inhibitors dronedarone or ketoconazole: Consider reducing the dose (see Dosage Modifications)
- CrCl 30-50 mL/min: Use of the P-gp inhibitors verapamil, amiodarone, quinidine, clarithromycin, and ticagrelor does not require a dose adjustment, however, these results should not be extrapolated to other P-gp inhibitors
- CrCl <30 mL/min: Avoid coadministration with all P-gp inhibitors
Reversing anticoagulant effect
- Idarucizumab is commercially available for reversal of the anticoagulant effect of dabigatran in adults for surgery/urgent procedures, or life-threatening or uncontrolled bleeding
- Can be dialyzed (protein binding is low, with the removal of about 60% of drug over 2-3 hr); however, the amount of data supporting this approach is limited
- Activated prothrombin complex concentrates, recombinant factor VIIa, or concentrates of coagulation factors II, IX, or X may be considered, but their use has not been evaluated in clinical trials
- Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of dabigatran
- Consider administration of platelet concentrates in cases in which thrombocytopenia is present or long-acting antiplatelet drugs have been used
- Efficacy and safety of idarucizumab not established in pediatric patients
Pregnancy & Lactation
Pregnancy
Limited available data on use in pregnant females are insufficient to determine drug-associated risks for adverse developmental outcomes; there are risks to mother associated with untreated venous thromboembolism in pregnancy and a risk of hemorrhage in mother and fetus associated with use of anticoagulants
Clinical considerations
- Pregnancy confers an increased risk for thromboembolism that is higher for females with underlying thromboembolic disease and certain high-risk pregnancy conditions; published data describe that women with previous history of venous thrombosis are at high risk for recurrence during pregnancy
- Use of anticoagulants, may increase risk of bleeding in fetus and neonate; monitor neonates for bleeding
Labor or delivery
- All patients receiving anticoagulants, including pregnant women, are at risk for bleeding; use during labor or delivery in women who are receiving neuraxial anesthesia may result in epidural or spinal hematomas; consider discontinuation or use of shorter acting anticoagulant as delivery approaches
Females of reproductive potential
- Females of reproductive potential requiring anticoagulation should discuss pregnancy planning with their physician
- The risk of clinically significant uterine bleeding, potentially requiring gynecological surgical interventions, identified with oral anticoagulants should be assessed in females of reproductive potential and those with abnormal uterine bleeding
Lactation
There are no data on presence of dabigatran in human milk, effects on breastfed child, or on milk production; drug and/or its metabolites were present in rat milk; breastfeeding is not recommended during therapy
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of Action
Prevents thrombus development through direct, competitive inhibition of thrombin (thrombin enables fibrinogen conversion to fibrin during the coagulation cascade)
Inhibits free and clot-bound thrombin and thrombin-induced platelet aggregation
Absorption
Peak plasma time: 1 hr (fasting); ~2 hr (high-fat meal)
Bioavailability
- Intact oral capsule: 3-7%; oral bioavailability increases by 75% when pellets are taken without the capsule shell
- Oral pellets: 37% higher relative bioavailability in healthy adults compared to dabigatran capsules
- Relative bioavailability between the 2 dosage forms is age dependent; relative bioavailability observed in adults cannot be translated to pediatric patients
Distribution
Protein bound: 35%
Vd: 50-70 L
Metabolism
Prodrug dabigatran etexilate is converted to dabigatran
Substrate of efflux transporter P-gp
Not a substrate, inhibitor, or inducer of CYP450 enzymes
Elimination
Half-life
- Pellets: 9-11 hr
-
Capsule
- Normal renal function: 12-17 hr
- Mild to moderate renal impairment: 14-17 hr
- Severe renal impairment: 28 hr
Renal clerance: 80% of total clearance after IV administration
Excretion: 7% urine; 86% feces
Administration
Oral Pellet Preparation
Administer only with specific soft foods or apple juice
Soft food preparation
- Mix with 2 teaspoons of following foods at room temperature
- Baby rice cereal prepared with water
- Mashed carrots
- Applesauce
- Mashed banana
Oral Administration
Oral capsules
- For adults and children aged 8 years to <18 years
- Swallow capsule whole (do not chew, crush, or break); do not open capsules and empty the pellets from the capsule
-
Missed dose
- If dose missed, take as soon as possible on same day
- Skip missed dose if unable to take at least 6 hr before next scheduled dose; do not double dose to make up for a missed dose
Oral pellets
- For pediatric patients aged 3 months to <12 years as soon as they are able to swallow soft food
- Administered twice daily, 1 dose in the morning and 1 dose in the evening, at approximately the same time every day; dosing interval should be as close to 12 hr as possible
- Give prepared medication before meals to ensure patient takes the full dose
- Administer immediately after mixing or within 30 minutes after mixing; discard if not administered within 30 minutes of mixing and prepare a new dose
- Administration with apple juice: Spoon oral pellets directly into patient’s mouth and swallow with apple juice or added to ~1-2 ounces of apple juice for drinking
-
Do not administer pellets
- Via syringes or feeding tubes
- With milk, milk products, or soft foods containing mild products
-
Missed or partial dose
- If dose missed, take as soon as possible on the same day
- Skip missed dose if unable to take at least 6 hr before next scheduled dose; do not double dose to make up for a missed dose
- If partial dose taken, do not administer a second dose at that time; administer next dose as scheduled ~12 hr later
Storage
Store at room temperature of 20-25ºC (68-77ºF); excursions permitted to 15-30ºC (59-86ºF)
Capsules: Store in original container; once bottle is opened, capsules are stable for only 4 months
Pellets: Store in original package to protect from moisture; do not open the packets until ready for use; use within 6 months of opening the aluminum bag containing the packets
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| dabigatran etexilate oral - | 150 mg capsule |  | |
| dabigatran etexilate oral - | 75 mg capsule |  | |
| dabigatran etexilate oral - | 150 mg capsule |  | |
| Pradaxa oral - | 150 mg capsule |  | |
| Pradaxa oral - | 75 mg capsule | 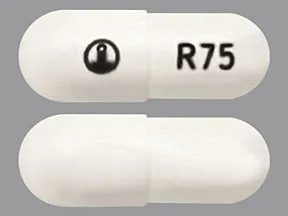 | |
| Pradaxa oral - | 110 mg capsule |  |
Copyright © 2010 First DataBank, Inc.
Patient Handout
dabigatran etexilate oral
DABIGATRAN PELLETS - ORAL
(DA-bi-GAT-ran)
COMMON BRAND NAME(S): Pradaxa
WARNING: Do not stop dabigatran unless directed by your child's doctor. If you stop giving this medication early, your child has a higher risk of forming a serious blood clot (such as stroke, blood clot in the legs/lungs). The doctor may direct your child to take a different "blood thinning" or antiplatelet medication to reduce your child's risk. Get medical help right away if your child has weakness on one side of the body, trouble speaking, sudden vision changes, confusion, chest pain, trouble breathing, or pain/warmth/swelling in the legs.People taking this medication may bleed near the spinal cord after certain spinal procedures. Bleeding in this area can cause paralysis that lasts a long time or could become permanent. Before any spinal procedure, ask the doctor about the benefits and risks. The risk of bleeding may be higher if your child has a deformed spine, or has had spinal procedures/surgery before (such as epidural catheter placement, difficult epidural/spinal puncture), or if your child is taking other drugs that can cause bleeding/bruising (including antiplatelet drugs such as clopidogrel, "blood thinners" such as warfarin/enoxaparin, nonsteroidal anti-inflammatory drugs-NSAIDs such as ibuprofen). Tell the doctor right away if you notice symptoms such as back pain, leg numbness/tingling/weakness, loss of control of the bowels or bladder (incontinence).
USES: This form of dabigatran is given to infants and children to treat blood clots in the veins of the legs (deep vein thrombosis) or lungs (pulmonary embolism) and to reduce the risk of them occurring again. Dabigatran is an anticoagulant that works by blocking certain clotting proteins in the blood. This helps to keep blood flowing smoothly in your child's body.Dabigatran should not be used to prevent blood clots from forming after artificial heart valve replacement. If your child had heart valve surgery, talk to the doctor about the best medication for your child.
HOW TO USE: See also Warning section.Read the Medication Guide and, if available, the Instructions for Use provided by the pharmacist before your child starts dabigatran and each time you get a refill. If you have any questions, ask the doctor or pharmacist.This medication is taken by mouth with or without food as directed by the doctor, usually twice daily. For the best effect, give this medication about 12 hours apart (first dose in the morning and second dose in the evening). To help you remember, give this medication at the same times every day.The dosage is based on your child's medical condition, age, weight, response to treatment, and other medications your child may be taking. Be sure to tell the doctor and pharmacist about all the products your child uses (including prescription drugs, nonprescription drugs, and herbal products).To give this medication without food, open the packet and spoon the contents into your child's mouth. Offer apple juice as needed to ensure the entire dose is swallowed. Pellets can also be mixed in a cup with a small amount of apple juice (such as 1 to 2 ounces/30 to 60 milliliters). If any pellets remain in the cup after drinking, add more apple juice to make sure the entire dose is taken.If you are mixing the pellets with soft food, open the packet and pour its contents into a small bowl with 2 teaspoons (10 milliliters) of certain soft foods (mashed carrots/banana or applesauce). The soft food should be at or below room temperature. Mix well with a spoon and give all of the mixture right away.Repeat these steps if the dose is for more than one packet. Do not give/mix with milk or milk products. Discard mixture after 30 minutes and do not save for later use. Do not prepare a supply in advance. Do not give using a syringe or feeding tube. If only part of the dose is taken, do not give another dose to catch up. Give the next dose at the regular time. Giving the medication before meals/feedings may help make sure your child will take the entire dose.It is very important to give it exactly as directed. Do not increase the dose or give this drug more often or for longer than prescribed. Your child's condition will not improve any faster, and the risk of serious side effects will increase.
SIDE EFFECTS: See also Warning section.Easy bruising, minor bleeding (such as nosebleed, bleeding from cuts), diarrhea, upset stomach, or heartburn may occur. If any of these effects last or get worse, tell the doctor or pharmacist promptly.Remember that this medication has been prescribed because the doctor has judged that the benefit to your child is greater than the risk of side effects. Many people using this medication do not have serious side effects.This medication can cause serious bleeding if it affects the blood clotting proteins too much. Tell the doctor right away if your child has any signs of serious bleeding, including: nosebleeds that happen often or don't stop, unusual tiredness/weakness, unusual pain/swelling/discomfort, unusual/easy bruising, prolonged bleeding from cuts or gums, unusually heavy/prolonged menstrual flow, pink/dark urine, coughing up blood, vomit that is bloody or looks like coffee grounds, severe headache, dizziness/fainting, bloody/black/tarry stools.Get medical help right away if your child has any signs of very serious bleeding, including: vision changes, confusion, trouble speaking, weakness on one side of the body.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact the doctor or pharmacist.In the US -Call the doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call the doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before giving dabigatran, tell the doctor or pharmacist if your child is allergic to it; or if your child has any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to the pharmacist for more details.Before using this medication, tell the doctor or pharmacist your child's medical history, especially of: mechanical heart valve, kidney disease, bleeding problems (such as bleeding of the stomach/intestines, bleeding in the brain), blood disorders (such as anemia, hemophilia, thrombocytopenia), liver disease, recent major injury/surgery, stroke, a certain clotting disorder (antiphospholipid syndrome), frequent falls/injuries.Before your child has surgery or any medical/dental procedures (especially spinal puncture or spinal/epidural anesthesia), tell the doctor or dentist that your child is taking this medication and about all the products your child uses (including prescription drugs, nonprescription drugs, and herbal products). The doctor or dentist may tell you to stop giving dabigatran before your surgery. Ask for specific instructions about stopping or starting this medication.This medication may cause stomach bleeding. Daily use of alcohol while using this medicine may increase the risk for stomach bleeding. Avoid alcoholic beverages.This medication can cause heavy bleeding. To lower the chance of getting cut, bruised, or injured, use caution with sharp objects like razors and nail cutters, and avoid activities such as contact sports. Your child should use an electric razor when shaving and a soft toothbrush when brushing their teeth. If your child falls or is injured, especially if your child hits their head, call the doctor right away. The doctor may need to check your child.This form of dabigatran is not usually used by adults. It is unlikely to be used during pregnancy or breastfeeding. Consult the doctor if you have any questions about this medication.
DRUG INTERACTIONS: See also Warning section.Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.Some products that may interact with this drug are: mifepristone, other drugs that can cause bleeding/bruising (including antiplatelet drugs such as clopidogrel, NSAIDs such as ibuprofen/naproxen, "blood thinners" such as warfarin/apixaban).Aspirin can increase the risk of bleeding when used with this medication. However, if the doctor has told you to give aspirin, your child should keep taking the aspirin unless the doctor tells you not to. Ask the doctor or pharmacist for more details.Other medications can affect the removal of dabigatran from the body, which may affect how dabigatran works. Examples include cobicistat, cyclosporine, dronedarone, ketoconazole, rifampin, St. John's wort, drugs used to treat seizures (such as carbamazepine, phenytoin), among others.
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call 1-800-222-1222. Canada residents can call 1-844-764-7669. Symptoms of overdose may include: bloody/black/tarry stools, pink/dark urine, unusual/prolonged bleeding.
NOTES: Do not share this medication with others.Lab and/or medical tests (such as kidney/liver function, clotting times) may be done while your child is taking this medication. Keep all medical and lab appointments. Consult the doctor for more details.
MISSED DOSE: If your child misses a dose, give it as soon as you remember. If it is less than 6 hours before the next dose, skip the missed dose. Give the next dose at the regular time. Do not double the dose to catch up.
STORAGE: Store at room temperature away from light and moisture. Do not store in the bathroom. Keep the packets in the aluminum bag until you are ready to give the medication. After opening the aluminum bag, discard the desiccant found in the bag. The packets must be used within 6 months of opening the aluminum bag. Discard any unused packets after 6 months. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
MEDICAL ALERT: Your child's condition can cause complications in a medical emergency. For information about enrolling in MedicAlert, call 1-888-633-4298 (US) or 1-800-668-1507 (Canada).
Information last revised May 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.







