Dosing & Uses
Dosage Forms & Strengths
powder for injection
- 5mg/vial (discontinued)
tablet
- 1mg
- 2mg
- 2.5mg
- 3mg
- 4mg
- 5mg
- 6mg
- 7.5mg
- 10mg
Venous Thrombosis
Prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism (PE)
Initial dose: 2-5 mg PO/IV qDay for 2 days, OR 10 mg PO for 2 days in healthy individuals
Initiate warfarin on day 1 or 2 of LMWH or unfractionated heparin therapy and overlap until desired INR, THEN discontinue heparin
Check INR after 2 days and adjust dose according to results
Typical maintenance dose ranges between 2 and 10 mg/day
Consider dosage based on genotype (see Genomic Considerations)
DVT and PE treatment
- Initiate warfarin on day 1 or 2 of parenteral anticoagulation therapy (eg, LMWH or unfractionated heparin)
- Overlap warfarin and parenteral anticoagulant for at least 5 days until desired INR (>2.0) maintained for 24 hours, then discontinue parenteral therapy
INR range and treatment duration
- Maintain an INR of 2.0-3.0
- Surgery-provoked DVT or PE: Treatment duration of 3 months
- Transient (reversible) risk factor-induced DVT or PE: Treatment duration of 3 months
- First unprovoked proximal DVT or PE with low or moderate bleeding risk: Extended treatment consideration with periodic (ie, annual) risk-benefit analysis
- First unprovoked proximal DVT or PE with high bleeding risk: Treatment duration of 3 months
- First unprovoked distal DVT regardless of bleeding risk: Treatment duration of 3 months
- Second unprovoked DVT or PE with low or moderate bleeding risk: Extended treatment
- Second unprovoked DVT or PE with high bleeding risk: Treatment duration of 3 months
- DVT/PE and active cancer: Extended treatment, with periodic risk-benefit analysis (ACCP recommends LMWH over vitamin K antagonist therapy)
- Prevention of venous thromboembolism for total knee arthroplasty, total hip arthroplasty, and hip fracture surgery: Minimum treatment duration of 10-14 days, with a recommendation to extend outpatient therapy to 35 days (ACCP recommends LMWH over vitamin K antagonist therapy)
Stroke & Thromboembolism
Prophylaxis and treatment of systemic embolic complications (eg, stroke) associated with atrial fibrillation (AF)
Initial dose: 2-5 mg PO/IV qDay × 2 days, OR 10 mg PO × 2 days in healthy individuals
Check INR after 2 days and adjust dose according to results
Typical maintenance dose ranges between 2-10 mg/day
Consider dosage based on genotype (see Genomic Considerations)
ACCP guidelines recommend dabigatran 150 mg PO BID over adjusted-dose warfarin therapy for AF unless both AF and mitral stenosis are present
INR range and treatment duration
- Nonvalvular AF: Maintain an INR of 2.0-3.0
- AF and stable CAD: Adjusted-dose warfarin therapy (INR 2.0-3.0) without aspirin
- AF with high stroke risk and placement of stent: Triple therapy of dose-adjusted warfarin (INR 2.0-3.0), clopidogrel, and aspirin; for 1 month if bare metal stent; for 3-6 months for drug-eluting stent
- AF with intermediate to high stroke risk without stent placement: 12 months of warfarin therapy (INR 2.0-3.0) with single antiplatelet regimen
- AF for more than 48 hours to undergo cardioversion: Warfarin therapy (INR 2.0-3.0) for 3 weeks prior to and 4 weeks after cardioversion
Indications for indefinite treatment duration
- Persistent or paroxysmal nonvalvular AF in patients with a high risk of stroke: Ie, patients who have risk factors for stroke, such as prior ischemic stroke, transient ischemic attack, or systemic embolism or who have 2 of the following risk factors--age greater than 75 years, moderately or severely impaired left ventricular systolic function and/or heart failure, history of hypertension, or diabetes mellitus
- Persistent or paroxysmal nonvalvular AF in patients with an intermediate risk of ischemic stroke: Ie, patients who have 1 of the following risk factors--age >75 years, moderately or severely impaired left ventricular systolic function and/or heart failure, history of hypertension, or diabetes mellitus
- AF and mitral stenosis
- ≥2 episodes of documented DVT or PE
Cardiac Valve Replacement
Prophylaxis and treatment of thromboembolic complications associated with cardiac valve replacement
Initial dose: 2-5 mg PO/IV qDay × 2 days, OR 10 mg PO × 2 days in healthy individuals
Check INR after 2 days and adjust dose according to results
Typical maintenance dose ranges between 2 and 10 mg/day
Consider dosage based on genotype (see Genomic Considerations)
INR and treatment duration
- Mitral bioprosthetic valve: INR 2.0-3.0 for a 3-month treatment duration; if other risk factors for thromboembolism are present (ie, AF, previous thromboembolism, left ventricular dysfunction), a longer duration may be necessary
- Aortic mechanical valve: INR 2.0-3.0 for indefinite treatment duration
- Mitral mechanical valve, caged ball or caged disk valve, or both aortic and mitral mechanical valves: INR 2.5-3.5 for indefinite treatment duration
- Mechanical valves include bileaflet mechanical valves and Medtronic Hall tilting disk valves
Post-Myocardial Infarction
Reduction in the risk of death, recurrent MI, and thromboembolic events (eg, stroke, systemic embolization) after MI
Initial dose: 2-5 mg PO/IV qDay × 2 days, OR 10 mg PO × 2 days in healthy individuals
Check INR after 2 days and adjust dose according to results
Typical maintenance dose ranges between 2 and 10 mg/day
Consider dosage based on genotype (see Genomic Considerations)
INR and treatment duration
- Maintain INR between 2.0 and 3.0
- In patients who have not had stenting and who have anterior MI and left ventricular (LV) thrombus or high risk of LV thrombus (ie, ejection fraction <40%, anteroapical wall-motion abnormality), treatment involves dual therapy of warfarin (INR 2.0-3.0) and low-dose aspirin 75-100 mg, daily; treatment duration is 3 months, after which warfarin is discontinued
- In patients who have had bare-metal stent placement and who have anterior MI and LV thrombus or high risk of LV thrombus (ejection fraction <40%, anteroapical wall-motion abnormality), treatment involves triple therapy of warfarin (INR 2.0-3.0), low-dose aspirin, and clopidogrel 75 mg, daily for 1 month, followed by warfarin (INR 2.0-3.0) and single antiplatelet therapy for second and third month, after which warfarin is discontinued
- In patients who have had drug-eluting stent placement and who have anterior MI and LV thrombus or high risk of LV thrombus (ejection fraction <40%, anteroapical wall-motion abnormality), treatment involves triple therapy of warfarin (INR 2.0-3.0), low-dose aspirin, and clopidogrel 75 mg, daily for 3-6 months, after which warfarin is discontinued
Rheumatic Valve Disease (Off-label)
Rheumatic valve disease with any of the following: Atrial diameter >55 mm, left atrial thrombus, atrial fibrillation, and previous systemic embolism
Maintain INR 2.0-3.0 indefinitely
Cryptogenic Stroke and Patent Foramen Ovale With DVT (Off-label)
Maintain INR between 2.0 and 3.0 for 3 months
Cardioembolic Stroke or TIA (Off-label)
Maintain INR between 2.0 and 3.0 indefinitely
ACCP guidelines recommend dabigatran 150 mg PO twice daily over dose-adjusted warfarin therapy
Systolic LV Dysfunction (Off-label)
Systolic LV dysfunction without established CAD but with identified acute LV thrombus (eg, Takotsubo cardiomyopathy)
Maintain INR between 2.0 and 3.0 for at least 3 months
Antiphospholipid Antibody Syndrome (Off-label)
Antiphospholipid antibody syndrome with previous arterial or venous thromboembolism
Maintain INR between 2.0 and 3.0 indefinitely
Genomic Considerations
ACCP 2012 guidelines recommend against using pharmacogenetic testing for guiding doses
CYP2C9 and vitamin K epoxide reductase complex, subunit 1 (VKORC1) genotype information can assist in selecting starting dose
If genotype information unavailable, usual starting dose is 2-5 mg/day (modify based on other patient factors)
Range of expected therapeutic doses based on CYP2C9 and VKORC1 genotypes are listed below
VKORC1-GG
- CYP2C9 *1/*1: 5-7 mg
- CYP2C9 *1/*2: 5-7 mg
- CYP2C9 *1/*3: 3-4 mg
- CYP2C9 *2/*2: 3-4 mg
- CYP2C9 *2/*3: 3-4 mg
- CYP2C9 *3/*3: 0.5-2 mg
VKORC1-AG
- CYP2C9 *1/*1: 5-7 mg
- CYP2C9 *1/*2: 3-4 mg
- CYP2C9 *1/*3: 3-4 mg
- CYP2C9 *2/*2: 3-4 mg
- CYP2C9 *2/*3: 0.5-2 mg
- CYP2C9 *3/*3: 0.5-2 mg
VKORC1-AA
- CYP2C9 *1/*1: 3-4 mg
- CYP2C9 *1/*2: 3-4 mg
- CYP2C9 *1/*3: 0.5-2 mg
- CYP2C9 *2/*2: 0.5-2 mg
- CYP2C9 *2/*3: 0.5-2 mg
- CYP2C9 *3/*3: 0.5-2 mg
Dosage Modifications
Hepatic impairment: May potentiate warfarin response because of decreased metabolism and impaired synthesis of clotting factors
Dosing Considerations
Indication determines intensity and duration of therapy
Individualized doses and monitoring of PT/INR are necessary
Monitoring frequency should be daily or once every few days until stabilized; once stable, q4-6 weeks or longer may be appropriate (eg, 12 weeks)
Not all factors causing warfarin dose variability are known, but they include age, race, sex, body weight, concomitant medications, and comorbidities, in addition to genetic factors
Lower starting doses (ie, 2-5 mg/day × 2 days) recommended with the elderly, hepatic impairment, poor nutrition, CHF, high bleeding risk, debilitated patients, heart valve replacement, concomitant medications known to increase warfarin effect, or individuals suspected of having genomic variants
Perioperative management recommendations: Hold warfarin therapy approximately 5 days before surgery; resume warfarin 12-24 hr after surgery; bridge anticoagulation during interruption in patients at high thromboembolism risk
Minor procedures and dental procedures: See ACCP guidelines for specific recommendations
Warfarin has no direct effect on an established thrombus, nor does it reverse ischemic tissue damage
Systemic atheroemboli and cholesterol microemboli; some cases have progressed to necrosis or death; discontinue therapy if such emboli occur
Pregnant women with mechanical heart valves: Therapy may cause fetal harm; however, benefits may outweigh the risks
Dosage Forms & Strengths
powder for injection
- 5mg/vial (discontinued)
tablets
- 1mg
- 2mg
- 2.5mg
- 3mg
- 4mg
- 5mg
- 6mg
- 7.5mg
- 10mg
Thrombosis
Prevention/treatment: If baseline INR is 1.0-1.3, administer loading dose of 0.1-0.2 mg/kg PO qDay × 1 day; check INR on days 2-4 and adjust daily dose to maintain INR between 2.0 and 3.0 (unless valve replacement indicates a higher range)
Use 0.1 mg/kg to initiate therapy with liver impairment or in patients who have had a Fontan procedure
Typical maintenance dose: 0.09-0.33 mg/kg/day, with infants <12 months old often requiring doses at high end of range
Dosing considerations
- Consistent anticoagulation in children is difficult and requires close supervision and frequent dose adjustments
- Refer to ACCP recommendations or institutional protocol for treatment duration dependent on indication
- Infants and children receiving vitamin K-supplemented nutrition (including infant formulas): May be resistant to warfarin therapy
- Infants with human-milk diet: May be sensitive to warfarin therapy
Dosing Considerations
Hepatic impairment
- Hepatic impairment may potentiate warfarin response because of decreased metabolism and impaired synthesis of clotting factors
- Load: 0.1 mg/kg PO qDay × 2 days
- Typical maintenance dose: 0.1 mg/kg PO qDay; adjust dose to achieve desired INR
- Common maintenance dose range: 0.05-0.34 mg/kg PO qDay
Anticoagulation
Lower doses required to produce therapeutic level of anticoagulation
Initial: ≤5 mg PO qDay
Maintenance: 2-5 mg PO qDay
Dosing Considerations
Elderly show greater than expected PT/INR response to anticoagulant effects of warfarin, possibly because of decreased hepatic function resulting in decreased warfarin metabolism and impaired synthesis of clotting factors
Caution should be used in elderly individuals who have increased risk of hemorrhage
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (3)
- defibrotide
defibrotide, warfarin. Either increases effects of the other by pharmacodynamic synergism. Contraindicated. Defibrotide is contraindicated with systemic anticoagulants. .
- mifepristone
mifepristone increases effects of warfarin by anticoagulation. Contraindicated.
- omacetaxine
omacetaxine increases effects of warfarin by anticoagulation. Contraindicated.
Serious - Use Alternative (24)
- adagrasib
adagrasib will increase the level or effect of warfarin by Other (see comment). Avoid or Use Alternate Drug. Avoid coadministration of adagrasib, a CYP3A4 and CYP2C9 inhibitor, with warfarin, a sensitive CYP3A and CYP2C9 substrate, unless otherwise recommended in the prescribing information for warfarin.
- allopurinol
allopurinol increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- apixaban
apixaban increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- argatroban
argatroban increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- betrixaban
betrixaban increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- bismuth subsalicylate
bismuth subsalicylate increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- bivalirudin
bivalirudin increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- cholestyramine
cholestyramine decreases effects of warfarin by inhibition of GI absorption. Applies only to oral form of both agents. Avoid or Use Alternate Drug. Cholestyramine and vitamin K antagonists should be administered 3-4 hr apart and monitor patients closely for reduced vitamin K antagonist effects.
- choline magnesium trisalicylate
choline magnesium trisalicylate increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- cimetidine
cimetidine increases effects of warfarin by unspecified interaction mechanism. Avoid or Use Alternate Drug.
- dabigatran
dabigatran increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- danazol
danazol increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- edoxaban
edoxaban increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- fluoxymesterone
fluoxymesterone increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- fondaparinux
fondaparinux increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- heparin
heparin increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- magnesium salicylate
magnesium salicylate increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- methyltestosterone
methyltestosterone increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- olutasidenib
olutasidenib will decrease the level or effect of warfarin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olutasidenib (a CYP3A4 inducer) with sensitive CYP3A substrates unless otherwise instructed in substrates prescribing information. If unavoidable, monitor for loss of therapeutic effect of sensitive CYP3A4 substrates.
- oxandrolone
oxandrolone increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- oxymetholone
oxymetholone increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- rivaroxaban
rivaroxaban increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug. Avoid combined use once INR is established in the desired therapeutic range.
- testosterone
testosterone increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
- vorapaxar
vorapaxar increases effects of warfarin by anticoagulation. Avoid or Use Alternate Drug.
Monitor Closely (298)
- abciximab
abciximab, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- acalabrutinib
acalabrutinib increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- acetaminophen
acetaminophen increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- acetaminophen IV
acetaminophen IV increases effects of warfarin by anticoagulation. Use Caution/Monitor. Likely to occur at doses exceedin 1.3-2 g/day for multiple consecutive days.
- acetaminophen rectal
acetaminophen rectal increases effects of warfarin by anticoagulation. Use Caution/Monitor. Likely to occur at doses exceedin 1.3-2 g/day for multiple consecutive days.
- acetaminophen/pamabrom
acetaminophen/pamabrom increases effects of warfarin by anticoagulation. Use Caution/Monitor. Likely to occur at doses exceedin 1.3-2 g/day acetaminophen for multiple consecutive days.
- acetaminophen/phenyltoloxamine
acetaminophen/phenyltoloxamine increases effects of warfarin by anticoagulation. Use Caution/Monitor. Likely to occur at doses exceedin 1.3-2 g/day acetaminophen for multiple consecutive days.
- alpelisib
alpelisib will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- aminosalicylic acid
aminosalicylic acid increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- amiodarone
amiodarone will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Coadministration increases INR by 100% after 3-4 days. Reduce warfarin dose by one-third to one-half and monitor INR.
- amitriptyline
amitriptyline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- amobarbital
amobarbital will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- anagrelide
anagrelide, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- apalutamide
apalutamide will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- aprepitant
aprepitant will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. In patients on chronic warfarin therapy, monitor INR in the 2-week period, particularly at 7-10 days, following aprepitant or fosaprepitant administration with each chemotherapy cycle
- armodafinil
armodafinil will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- asciminib
asciminib will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
- aspirin
aspirin increases effects of warfarin by anticoagulation. Modify Therapy/Monitor Closely. Avoid coadministration of chronic high-dose aspirin. Aspirin's antiplatelet properties may increase anticoagulation effect of warfarin. The need for simultaneous use of low-dose aspirin and warfarin is common for patients with cardiovascular disease. .
- atazanavir
atazanavir will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- atovaquone
atovaquone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- azathioprine
azathioprine decreases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- azithromycin
azithromycin increases toxicity of warfarin by anticoagulation. Use Caution/Monitor. Postmarketing reports have suggested that concomitant administration of azithromycin may potentiate effects of oral warfarin but the interaction does not appear to alter prothrombin time.
- balsalazide
balsalazide increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- belzutifan
belzutifan will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- benzhydrocodone/acetaminophen
benzhydrocodone/acetaminophen increases effects of warfarin by anticoagulation. Use Caution/Monitor. Likely to occur at doses exceedin 1.3-2 g/day acetamionphen for multiple consecutive days.
- betamethasone
betamethasone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- bexarotene
bexarotene will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- bicalutamide
bicalutamide increases effects of warfarin by Other (see comment). Use Caution/Monitor. Comment: May increase free concentrations of vitamin K antagonists.
- bosentan
bosentan will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- butalbital
butalbital will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- cangrelor
cangrelor, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- capecitabine
capecitabine will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Closely monitor INR and PT and adjust dose. Increased INR and PT can occur within a few days of initiating capecitabine.
- carbamazepine
carbamazepine will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- cefaclor
cefaclor increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefadroxil
cefadroxil increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefazolin
cefazolin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefdinir
cefdinir increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefditoren
cefditoren increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefepime
cefepime increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor. Cefepime may decrease prothrombin activity.
- cefepime/enmetazobactam
cefepime/enmetazobactam increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor. Cefepime/enmetazobactam may decrease prothrombin activity.
- cefiderocol
cefiderocol increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefixime
cefixime increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefotaxime
cefotaxime increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefotetan
cefotetan increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefoxitin
cefoxitin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefpodoxime
cefpodoxime increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefprozil
cefprozil increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ceftaroline
ceftaroline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ceftazidime
ceftazidime increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ceftibuten
ceftibuten increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ceftolozane/tazobactam
ceftolozane/tazobactam increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ceftriaxone
ceftriaxone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cefuroxime
cefuroxime increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- celecoxib
celecoxib increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- cenobamate
cenobamate will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- cephalexin
cephalexin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ceritinib
ceritinib will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
- chenodiol
chenodiol increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- chloral hydrate
chloral hydrate increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- chloramphenicol
chloramphenicol will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- chlorpropamide
chlorpropamide, warfarin. Either increases effects of the other by receptor binding competition. Use Caution/Monitor. Monitor for decreased vitamin K antagonist effects (eg, decreased INR, thrombosis) when combined with metformin. Additionally, consider increased monitoring for hypoglycemia with this combination. Competitive inhibition of CYP2C9-mediated metabolism may also contribute to mechanism.
- cilostazol
cilostazol, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- ciprofloxacin
ciprofloxacin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- citalopram
citalopram, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- clarithromycin
clarithromycin will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- clopidogrel
clopidogrel, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- cobicistat
cobicistat will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- coenzyme Q10
coenzyme Q10, warfarin. unspecified interaction mechanism. Use Caution/Monitor. The data from studies and case reports is conflicting.
- colesevelam
colesevelam increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- conivaptan
conivaptan will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- dabrafenib
dabrafenib will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
dabrafenib will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed. - darunavir
darunavir, warfarin. Other (see comment). Use Caution/Monitor. Comment: Warfarin serum concentrations may be increased or decreased. Darunavir may increase levels the less potent R-enantiomer of warfarin, but is used in combination with ritonavir which may decrease R-warfarin levels. .
- dasatinib
dasatinib increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- delafloxacin
delafloxacin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- delavirdine
delavirdine will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- demeclocycline
demeclocycline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- deoxycholic acid
deoxycholic acid increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- desogestrel
desogestrel increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- desvenlafaxine
desvenlafaxine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- diclofenac
diclofenac, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- dienogest/estradiol valerate
dienogest/estradiol valerate increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- diflunisal
diflunisal, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- dipyridamole
dipyridamole, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- doxycycline
doxycycline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- dronedarone
dronedarone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- drospirenone
drospirenone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- duloxetine
duloxetine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- econazole topical
econazole topical will increase the level or effect of warfarin by anticoagulation. Use Caution/Monitor. Most cases reported product application with use under occlusion, genital application, or application to a large body surface area which may increase systemic absorption; monitor International Normalized Ratio (INR) and/or prothrombin time, especially for patients who apply to large body surface areas, in the genital area, or under occlusion
- efavirenz
efavirenz will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- elagolix
elagolix will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- elranatamab
elranatamab will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Elranatamab causes cytokine release syndrome (CRS) that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. This is more likely to occur from initiation of elranatamab step-up dosing up to 14 days after the first treatment dose and during and after CRS.
- elvitegravir
elvitegravir will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- encorafenib
encorafenib, warfarin. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Warfarin serum concentrations may be increased or decreased. Encorafenib it both an inhibitor and inducer of CYP3A4. The less potent R-enantiomer of warfarin is a substrate of CYP3A4.
- entacapone
entacapone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- enzalutamide
enzalutamide will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- epcoritamab
epcoritamab, warfarin. affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Epcoritamab causes release of cytokines that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. For certain CYP substrates, minimal changes in their concentration may lead to serious adverse reactions. If needed, modify therapy as recommended in the substrate's prescribing information. .
- epoprostenol
epoprostenol, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- eptifibatide
eptifibatide, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- eravacycline
eravacycline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- escitalopram
escitalopram, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- eslicarbazepine acetate
eslicarbazepine acetate will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- estradiol
estradiol increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ethacrynic acid
ethacrynic acid increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- etodolac
etodolac, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- etoposide
etoposide increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- etravirine
etravirine will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
etravirine will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed. - exenatide injectable solution
exenatide injectable solution increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- exenatide injectable suspension
exenatide injectable suspension increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- exenatide subdermal implant
exenatide subdermal implant increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- fenofibrate
fenofibrate will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Mechanism of interaction may be caused by CYP2C9 inhibition and protein-binding displacement.
- fenofibrate micronized
fenofibrate micronized will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Mechanism of interaction may be caused by CYP2C9 inhibition and protein-binding displacement.
- fenofibric acid
fenofibric acid will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Mechanism of interaction may be caused by CYP2C9 inhibition and protein-binding displacement.
- fenoprofen
fenoprofen, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- fexinidazole
fexinidazole will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- fluconazole
fluconazole will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. If coadministered, consider decreasing warfarin dose by 10-20%.
- fludrocortisone
fludrocortisone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- fluorouracil
fluorouracil will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- fluoxetine
fluoxetine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- flurbiprofen
flurbiprofen will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
flurbiprofen, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin. - fluvastatin
fluvastatin will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
fluvastatin increases effects of warfarin by anticoagulation. Use Caution/Monitor. Dosage adjustment of anticoagulant based in INR and clinical response may be necessary. - fluvoxamine
fluvoxamine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- fosamprenavir
fosamprenavir will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- fosaprepitant
fosaprepitant will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. In patients on chronic warfarin therapy, monitor INR in the 2-week period, particularly at 7-10 days, following aprepitant or fosaprepitant administration with each chemotherapy cycle
- fosphenytoin
fosphenytoin will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- fruquintinib
fruquintinib, warfarin. Other (see comment). Use Caution/Monitor. Comment: Fruquintinib may cause serious hemorrhagic events. Monitor INR in patients receiving anticoagulants.
- garlic
garlic increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- gefitinib
gefitinib increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- gemcitabine
gemcitabine increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- gemfibrozil
gemfibrozil will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. If coadministered, consider decreasing warfarin dose by one-fourth to one-third.
- gemifloxacin
gemifloxacin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- givosiran
givosiran will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- glimepiride
glimepiride, warfarin. Either increases effects of the other by receptor binding competition. Use Caution/Monitor. Monitor for decreased vitamin K antagonist effects (eg, decreased INR, thrombosis) when combined with metformin. Additionally, consider increased monitoring for hypoglycemia with this combination. Competitive inhibition of CYP2C9-mediated metabolism may also contribute to mechanism.
- glipizide
glipizide, warfarin. Either increases effects of the other by receptor binding competition. Use Caution/Monitor. Monitor for decreased vitamin K antagonist effects (eg, decreased INR, thrombosis) when combined with metformin. Additionally, consider increased monitoring for hypoglycemia with this combination. Competitive inhibition of CYP2C9-mediated metabolism may also contribute to mechanism.
- glofitamab
glofitamab, warfarin. affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Glofitamab causes release of cytokines that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. For certain CYP substrates, minimal changes in their concentration may lead to serious adverse reactions. If needed, modify therapy as recommended in the substrate's prescribing information. .
- glucagon
glucagon increases effects of warfarin by Other (see comment). Use Caution/Monitor. Comment: Effect observed only when doses exceed 50 mg administered over a 2 day period.
- glyburide
glyburide, warfarin. Either increases effects of the other by receptor binding competition. Use Caution/Monitor. Monitor for decreased vitamin K antagonist effects (eg, decreased INR, thrombosis) when combined with metformin. Additionally, consider increased monitoring for hypoglycemia with this combination. Competitive inhibition of CYP2C9-mediated metabolism may also contribute to mechanism.
- griseofulvin
griseofulvin will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- hydrocortisone
hydrocortisone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ibritumomab tiuxetan
ibritumomab tiuxetan increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- ibrutinib
ibrutinib, warfarin. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Ibrutinib may potentiate the effects of anticoagulant agents such as warfarin may increase the risk of bleeding; monitor for signs of bleeding.
warfarin, ibrutinib. Either increases effects of the other by anticoagulation. Use Caution/Monitor. Ibrutinib may potentiate the effects of anticoagulant agents such as warfarin may increase the risk of bleeding; monitor for signs of bleeding. - ibuprofen
ibuprofen, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- ibuprofen IV
ibuprofen IV, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- icosapent
icosapent increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- idelalisib
idelalisib will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- iloprost inhaled
iloprost inhaled, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- indinavir
indinavir will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- indomethacin
indomethacin, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- inotersen
inotersen increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- interferon alfa 2b
interferon alfa 2b increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- interferon alfa n3
interferon alfa n3 increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- isoniazid
isoniazid will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- itraconazole
itraconazole will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- ivermectin
ivermectin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ivosidenib
ivosidenib will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- kanamycin
kanamycin increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- ketoconazole
ketoconazole will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- ketoprofen
ketoprofen, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- ketorolac
ketorolac, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- lactulose
lactulose increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- leflunomide
leflunomide increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- levocarnitine
levocarnitine increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- levofloxacin
levofloxacin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- levomilnacipran
levomilnacipran, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- levonorgestrel oral/ethinylestradiol/ferrous bisglycinate
levonorgestrel oral/ethinylestradiol/ferrous bisglycinate increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- levonorgestrel transdermal
levonorgestrel transdermal increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- levothyroxine
levothyroxine increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- liothyronine
liothyronine increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- liotrix
liotrix increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- lonafarnib
lonafarnib will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- lonapegsomatropin
lonapegsomatropin will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- lopinavir
lopinavir will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- lorlatinib
lorlatinib will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- losartan
losartan will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
- lovastatin
lovastatin increases effects of warfarin by anticoagulation. Use Caution/Monitor. Dosage adjustment of anticoagulant based in INR and clinical response may be necessary.
- lumacaftor/ivacaftor
lumacaftor/ivacaftor will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- meclofenamate
meclofenamate, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- mefenamic acid
mefenamic acid, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- mefloquine
mefloquine increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- megestrol
megestrol increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- meloxicam
meloxicam, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- mesalamine
mesalamine increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- methimazole
methimazole decreases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- methotrexate
methotrexate increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- methoxsalen
methoxsalen will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- methylphenidate
methylphenidate increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- methylphenidate transdermal
methylphenidate transdermal will increase the level or effect of warfarin by decreasing metabolism. Modify Therapy/Monitor Closely. Decreasing the dose of these drugs may be required when given coadministered with methylphenidate. Consider monitoring plasma drug concentrations (or INR with coumadin), when initiating or discontinuing methylphenidate.
- methylprednisolone
methylprednisolone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- metronidazole
metronidazole increases levels of warfarin by unspecified interaction mechanism. Use Caution/Monitor. Metronidazole may potentiate the anticoagulant effect of warfarin and other oral coumarin anticoagulants, resulting in a prolongation of prothrombin time. .
- mexiletine
mexiletine will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- mibefradil
mibefradil will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- miconazole oral
miconazole oral will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- milnacipran
milnacipran, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- minocycline
minocycline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- mitapivat
mitapivat will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- mitotane
mitotane will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- mobocertinib
mobocertinib will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- modafinil
modafinil will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- moxifloxacin
moxifloxacin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- nabumetone
nabumetone, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- nafcillin
nafcillin will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- naproxen
naproxen, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- nefazodone
nefazodone will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- nelfinavir
nelfinavir will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- neomycin PO
neomycin PO increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- nifedipine
nifedipine will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- nintedanib
nintedanib increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- nirmatrelvir/ritonavir
nirmatrelvir/ritonavir will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. INR may increase or decrease. Closely monitor INR if nirmatrelvir/ritonavir is coadministered with warfarin.
- nitisinone
nitisinone will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
- norgestimate
norgestimate increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- obinutuzumab
obinutuzumab increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- ofloxacin
ofloxacin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- olsalazine
olsalazine increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- omadacycline
omadacycline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- omaveloxolone
omaveloxolone will decrease the level or effect of warfarin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Omaveloxolone may reduce systemic exposure of sensitive CYP3A4 substrates. Check prescribing information of substrate if dosage modification is needed.
- omega 3 fatty acids
omega 3 fatty acids increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- omeprazole
omeprazole will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- orlistat
orlistat increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- oxaprozin
oxaprozin, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- paroxetine
paroxetine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- peginterferon alfa 2a
peginterferon alfa 2a increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- peginterferon alfa 2b
peginterferon alfa 2b increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- pentobarbital
pentobarbital will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- pentosan polysulfate sodium
pentosan polysulfate sodium increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- pentoxifylline
pentoxifylline increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- pexidartinib
pexidartinib will decrease the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inducers of these isoenzymes and adjust warfarin dose if needed.
- phenobarbital
phenobarbital will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- phenytoin
phenytoin will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- piperacillin
piperacillin, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Platelet dysfunction occurs with extended-spectrum penicillins in varying degrees. Monitor INR and adjust warfarin dose if needed.
- piroxicam
piroxicam, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- pirtobrutinib
pirtobrutinib will increase the level or effect of warfarin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Pirtobrutinib (a CYP3A4 inhibitor) may increase plasma concentrations of sensitive CYP3A4 substrate which may increase the risk of adverse reactions related to these substrates.
- posaconazole
posaconazole will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- potassium iodide
potassium iodide decreases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- prasugrel
prasugrel, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- pravastatin
pravastatin increases effects of warfarin by anticoagulation. Use Caution/Monitor. Dosage adjustment of anticoagulant based in INR and clinical response may be necessary.
- prednisolone
prednisolone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- prednisone
prednisone increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- primaquine
primaquine will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- primidone
primidone will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- propofol
propofol will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- propylthiouracil
propylthiouracil decreases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- quinidine
quinidine will increase the level or effect of warfarin by decreasing metabolism. Use Caution/Monitor. Cinchona alkaloids, including quinine and quinidine, may increase anticoagulant effect of vitamin K antagonists by inhibiting hepatic synthesis of vitamin K-dependent coagulation proteins.
- quinine
quinine will increase the level or effect of warfarin by decreasing metabolism. Use Caution/Monitor. Cinchona alkaloids, including quinine and quinidine, may increase anticoagulant effect of vitamin K antagonists by inhibiting hepatic synthesis of vitamin K-dependent coagulation proteins.
- regorafenib
regorafenib increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- remdesivir
remdesivir increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- reteplase
reteplase increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- rifampin
rifampin will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- rifapentine
rifapentine will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- ritlecitinib
ritlecitinib will increase the level or effect of warfarin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Ritlecitinib inhibits CYP3A4 substrates; coadministration increases AUC and peak plasma concentration sensitive substrates, which may increase risk of adverse reactions. Additional monitoring and dosage adjustment may be needed in accordance with product labeling of CYP3A substrates.
- ritonavir
ritonavir will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- romidepsin
romidepsin increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ropeginterferon alfa 2b
ropeginterferon alfa 2b increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- rosuvastatin
rosuvastatin increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- rucaparib
rucaparib will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Rucaparib inhibits CYP1A2, CYP3A (the less potent warfarin R-enantiomer is a substrates of these). Also inhibits CYP2C9, of which the more potent warfarin S-enantiomer is a substrate.
- saquinavir
saquinavir will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- secobarbital
secobarbital will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- segesterone/ethinyl estradiol
segesterone/ethinyl estradiol increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- sertraline
sertraline, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- simvastatin
simvastatin increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- somapacitan
somapacitan will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- somatrogon
somatrogon will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- somatropin
somatropin will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Limited published data indicate that growth hormone treatment increases cytochrome P450 (CYP450)-mediated antipyrine clearance. Caution with sensitive CYP substrates
- sorafenib
sorafenib will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
- sotorasib
sotorasib will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- sparsentan
sparsentan will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Sparsentan (a CYP2C9 inducer) decreases exposure of CYP2C9 substrates and reduces efficacy related to these substrates.
- St John's Wort
St John's Wort will decrease the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- sulfadiazine
sulfadiazine will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Mechanism of interaction may be caused by CYP2C9 inhibition and protein-binding displacement. If coadministered, consider decreasing warfarin dose by 10-20%.
- sulfamethoxazole
sulfamethoxazole will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely. Mechanism of interaction may be caused by CYP2C9 inhibition and protein-binding displacement. If coadministered, consider decreasing warfarin dose by 10-20%.
- sulfasalazine
sulfasalazine increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- sulindac
sulindac, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- talquetamab
talquetamab will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor. Talquetamab causes cytokine release syndrome (CRS) that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. This is more likely to occur from initiation of talquetamab step-up dosing up to 14 days after the first treatment dose and during and after CRS.
- teclistamab
teclistamab will increase the level or effect of warfarin by altering metabolism. Use Caution/Monitor. Teclistamab causes release of cytokines that may suppress activity of CYP450 enzymes, resulting in increased exposure of CYP substrates. Monitor for increased concentrations or toxicities of sensitive CYP substrates. Adjust dose of CYP substrate drug as needed.
- telavancin
telavancin increases effects of warfarin by anticoagulation. Use Caution/Monitor.
- tenecteplase
tenecteplase increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- tetracycline
tetracycline increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- thyroid desiccated
thyroid desiccated increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- ticagrelor
ticagrelor, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- ticarcillin
ticarcillin, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Platelet dysfunction occurs with extended-spectrum penicillins in varying degrees. Monitor INR and adjust warfarin dose if needed.
- ticlopidine
ticlopidine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
ticlopidine will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed. - tipranavir
tipranavir will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- tirofiban
tirofiban, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- tolazamide
tolazamide, warfarin. Either increases effects of the other by receptor binding competition. Use Caution/Monitor. Monitor for decreased vitamin K antagonist effects (eg, decreased INR, thrombosis) when combined with metformin. Additionally, consider increased monitoring for hypoglycemia with this combination. Competitive inhibition of CYP2C9-mediated metabolism may also contribute to mechanism.
- tolbutamide
tolbutamide, warfarin. Either increases effects of the other by receptor binding competition. Use Caution/Monitor. Monitor for decreased vitamin K antagonist effects (eg, decreased INR, thrombosis) when combined with metformin. Additionally, consider increased monitoring for hypoglycemia with this combination. Competitive inhibition of CYP2C9-mediated metabolism may also contribute to mechanism.
- tolmetin
tolmetin, warfarin. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Drugs with antiplatelet properties may increase anticoagulation effect of warfarin.
- toremifene
toremifene increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- tranylcypromine
tranylcypromine will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
- triamcinolone acetonide extended-release injectable suspension
triamcinolone acetonide extended-release injectable suspension increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- triamcinolone acetonide injectable suspension
triamcinolone acetonide injectable suspension increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- trofinetide
trofinetide will increase the level or effect of warfarin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Monitor CYP3A4 substrates for which a small increase in plasma concentration may lead to serious toxicities if coadministered with trofinetide (a weak CYP3A4 inhibitor).
- venlafaxine
venlafaxine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- vilazodone
vilazodone, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- vitamin A
vitamin A increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- vitamin E
vitamin E increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- vitamin K1 (phytonadione)
vitamin K1 (phytonadione), warfarin. Either decreases effects of the other by anticoagulation. Use Caution/Monitor. Monitor INR with corresponding increases or decreases in vitamin K intake significantly affecting vitamin k blood levels.
- voriconazole
voriconazole will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Modify Therapy/Monitor Closely.
- vortioxetine
vortioxetine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- zafirlukast
zafirlukast will increase the level or effect of warfarin by affecting hepatic enzyme CYP2C9/10 metabolism. Use Caution/Monitor.
- zanubrutinib
zanubrutinib increases effects of warfarin by unspecified interaction mechanism. Use Caution/Monitor.
- zileuton
zileuton will increase the level or effect of warfarin by Other (see comment). Use Caution/Monitor. Warfarin's less potent R-enantiomer is metabolized in part by CYP3A4 (and also CYP1A2 and CYP2C19). Monitor INR more frequently if coadministered with inhibitors of these isoenzymes and adjust warfarin dose if needed.
Minor (7)
- acetazolamide
warfarin will decrease the level or effect of acetazolamide by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- anastrozole
warfarin will decrease the level or effect of anastrozole by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- ceritinib
warfarin will decrease the level or effect of ceritinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- cyclophosphamide
warfarin will decrease the level or effect of cyclophosphamide by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- danazol
warfarin will decrease the level or effect of danazol by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- drospirenone
warfarin will decrease the level or effect of drospirenone by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- larotrectinib
warfarin will decrease the level or effect of larotrectinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
Adverse Effects
Frequency Not Defined
Cholesterol embolus syndrome
Intraocular hemorrhage
Abdominal pain
Flatulence
Alopecia
Rash
Pruritus
Taste disturbance
Tissue necrosis
Headache
Lethargy
Dizziness
Hematuria
Anemia
Hepatitis
Respiratory tract bleeding
Hypersensitivity reaction
Hemorrhage
Blood dyscrasias
Fever
"Purple toe" syndrome
Increased fracture risk with long-term usage
Calciphylaxis
Postmarketing Reports
Acute kidney injury
Limb ischemia, necrosis, and gangrene in patients with HIT and HITTS
Warnings
Black Box Warnings
Warfarin sodium can cause major or fatal bleeding; bleeding is more likely to occur during the starting period and with a higher dose (resulting in a higher INR)
Risk factors for bleeding include high intensity of anticoagulation (INR greater than 4), age 65 years or older, highly variable INRs, history of gastrointestinal bleeding, hypertension, cerebrovascular disease, serious heart disease, anemia, malignancy, trauma, renal insufficiency, concomitant drugs, and long duration of warfarin therapy
Regular monitoring of INR should be performed on all treated patients; those at high risk of bleeding may benefit from more frequent INR monitoring, careful dose adjustment to desired INR, and a shorter duration of therapy
Patients should be instructed about prevention measures to minimize the risk of bleeding and to immediately report any signs or symptoms of bleeding to their physician
Contraindications
Pregnancy, except in women with mechanical heart valves
Hemorrhagic tendencies or blood dyscrasias
Recent or contemplated CNS or eye surgery or traumatic surgery resulting in large open surfaces
Bleeding tendencies associated with CNS hemorrhage, cerebral aneurysms, dissecting aorta, pericarditis and pericardial effusions, bacterial endocarditis, and active ulceration or overt bleeding of the GI, GU, or respiratory tract
Threatened abortion, eclampsia, and preeclampsia
Unsupervised patients with conditions associated with potential high level of noncompliance (eg, dementia, alcoholism, psychosis)
Spinal puncture and other diagnostic or therapeutic procedures with potential for uncontrollable bleeding
Major regional or lumbar block anesthesia
Known hypersensitivity
Malignant hypertension
Cautions
Lower doses may be warranted in the elderly, debilitated patients, malnutrition, CHF, or liver disease
Elicits no direct effect on an established thrombus, nor does it reverse ischemic tissue damage
INR >4.0 appears to provide no additional therapeutic benefit in most patients and is associated with a higher risk of bleeding
Skin necrosis reported with use; caution in patients at risk for hemorrhage, necrosis, or gangrene
Heparin-induced thrombocytopenia, DVT (may defer warfarin until thrombin generation is controlled and thrombocytopenia has resolved)
Genetic tests may be warranted to determine best dose for individual patients; variations in CYP2C9 and VKORC1 genes may modify response
Advise patients receiving warfarin to carry a notice stating that they are undergoing anticoagulant therapy, to alert medical/emergency personnel
Use caution in patients with acute infection or active TB or conditions that may alter normal GI flora; antibiotics and fever may change response to warfarin
May release atheromatous plaque emboli; may experience symptoms depending on site of embolization common organs like pancreas, liver, kidneys, and spleen, which may lead to necrosis or death
Use caution in patients with prolonged vitamin K insufficiencies
Thyroid disease may increase warfarin responsiveness
May impair synthesis of coagulation factors in patients with reduced liver function, regardless of etiology, which in turn may lead to increased warfarin sensitivity
Use caution in lactation
Calciphylaxis or calcium uremic arteriolopathy has been reported in patients with and without end-stage renal disease; discontinue warfarin and treat calciphylaxis as appropriate; consider alternative anticoagulant therapy
Maintain consistent intake of vitamin K-containing foods; high vitamin K consumption may decrease warfarin effect
In patients with altered glomerular integrity or with history of kidney disease, acute kidney injury may occur with therapy, possibly in relation to episodes of excessive anticoagulation and hematuria; more frequent monitoring of anticoagulation is advised in patients with compromised renal function
Hepatic impairment may impair synthesis of clotting factors and decrease metabolism of warfarin; conduct more frequent monitoring for bleeding
Contraindicated in any unsupervised patient with senility; conduct more frequent monitoring for bleeding in elderly patients receiving therapy in any situation
Pregnancy & Lactation
Pregnancy
Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications; estimated background risk of major birth defects and miscarriage for indicated population is unknown
Exposure during pregnancy causes a recognized pattern of major congenital malformations (warfarin embryopathy and fetotoxicity), fatal fetal hemorrhage, and an increased risk of spontaneous abortion and fetal mortality
Verify pregnancy status of females of reproductive potential prior to initiating therapy
Advise females of reproductive potential to use effective contraception during treatment, and for at least 1 month after final dose of warfarin
Lactation
Not excreted in breast milk as reported in limited published study (AAP Committee states compatible with nursing); because of potential for serious adverse reactions, including bleeding in breastfed infant, consider developmental and health benefits of breastfeeding along with mother’s clinical need for therapy; monitor breastfeeding infants for bruising or bleeding
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of Action
Interferes with hepatic synthesis of vitamin K-dependent clotting factors II, VII, IX, and X, as well as proteins C and S; S-warfarin is 4 times more potent than R-warfarin
Warfarin depletes functional vitamin K reserves, which in turn reduces synthesis of active clotting factors, by competitively inhibiting subunit 1 of the multi-unit vitamin K epoxide reductase complex 1 (VKOR1)
Absorption
Onset: 36-48 hr
Duration: 2-5 days
Peak plasma time: 1.5-3 days
Distribution
Protein bound: 99% (albumin)
Vd: 0.14 L/kg
Metabolism
R-warfarin: Hepatic P450 enzymes CYP1A2, CYP2C19, CYP3A4
S-warfarin: CYP2C9
Elimination
Half-life: 20-60 hr (patient specific)
Pharmacogenomics
Metabolized primarily via oxidation in the liver by CYP2C9; exerts its anticoagulant effect by inhibiting the protein VKORC1
Dose influenced by genetic factors (CYP2C9, VKORC1 genotypes)
Carriers of CYP2C9*2 and CYP2C9*3 require ~19-33% dose reduction, respectively, per allele compared with persons who carry the *1 allele
Carriers of the VKORC1 A allele require ~28% dose reduction per allele in their genotype compared with persons who carry none
Genetic testing laboratories
- The following companies provide genetic testing for CYP2C9 and VKORC1 variants
- AutoGenomics (http://www.autogenomics.com)
- EntroGen (http://www.entrogen.com)
- Kimball Genetics (http://www.kimballgenetics.com)
- Nanosphere (http://www.nanosphere.us)
- Osmetech (http://www.osmetech.com)
- Specialty Laboratories (http://www.specialtylabs.com)
Administration
IV Incompatibilities
Solution: D10W, NS (?), LR (?)
Syringe: Heparin
Y-site: Aminophylline, NH4Cl (?), bretylium, ceftazidime, dobutamine, ciprofloxacin, cimetidine, esmolol, labetalol, metronidazole, Ringer's, vancomycin (may be compatible at low conc of warfarin), and promazine
IV Preparation
Reconstitute in 2.7 mL SWI to obtain 2 mg/mL injectable solution
Use reconstituted solution within 4 hr; discard unused portion
IV Administration
Inject 2 mg/mL solution slowly (over 1-2 min) into a peripheral vein
IV Storage
Store at room temp and protect from light
Do not refrigerate
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| Jantoven oral - | 10 mg tablet | 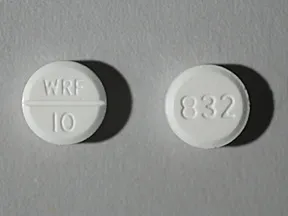 | |
| Jantoven oral - | 4 mg tablet |  | |
| Jantoven oral - | 3 mg tablet | 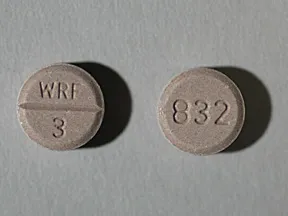 | |
| Jantoven oral - | 5 mg tablet |  | |
| Jantoven oral - | 7.5 mg tablet |  | |
| Jantoven oral - | 10 mg tablet | 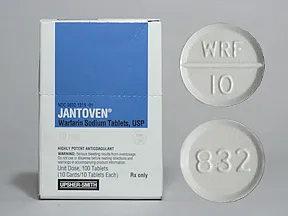 | |
| Jantoven oral - | 6 mg tablet | 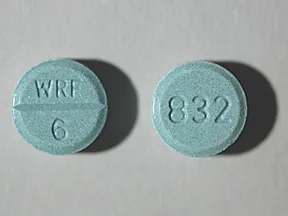 | |
| Jantoven oral - | 2.5 mg tablet |  | |
| Jantoven oral - | 2 mg tablet |  | |
| Jantoven oral - | 1 mg tablet | 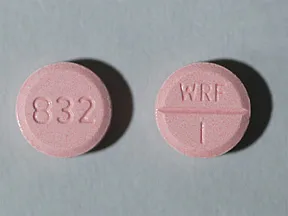 | |
| warfarin oral - | 4 mg tablet |  | |
| warfarin oral - | 5 mg tablet |  | |
| warfarin oral - | 2 mg tablet | 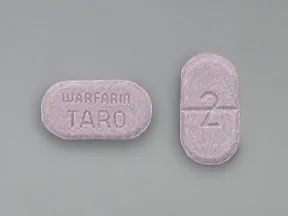 | |
| warfarin oral - | 5 mg tablet | 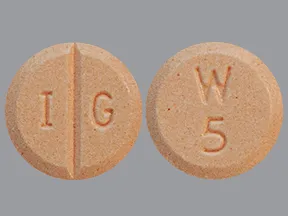 | |
| warfarin oral - | 6 mg tablet |  | |
| warfarin oral - | 3 mg tablet |  | |
| warfarin oral - | 2.5 mg tablet | 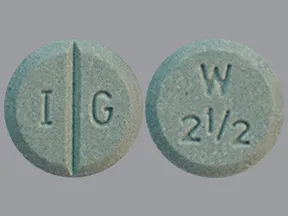 | |
| warfarin oral - | 4 mg tablet | 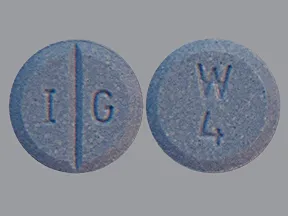 | |
| warfarin oral - | 2 mg tablet | 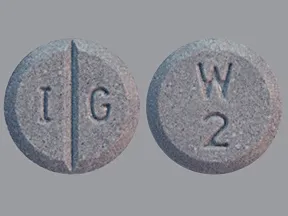 | |
| warfarin oral - | 1 mg tablet |  | |
| warfarin oral - | 5 mg tablet |  | |
| warfarin oral - | 1 mg tablet | 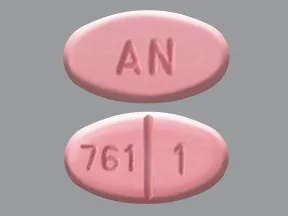 | |
| warfarin oral - | 4 mg tablet | 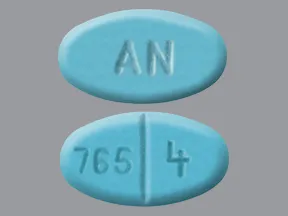 | |
| warfarin oral - | 10 mg tablet | 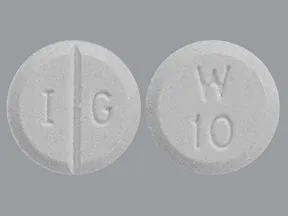 | |
| warfarin oral - | 6 mg tablet | 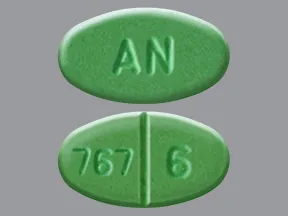 | |
| warfarin oral - | 3 mg tablet | 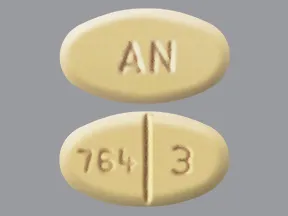 | |
| warfarin oral - | 2 mg tablet | 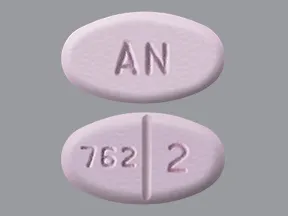 | |
| warfarin oral - | 5 mg tablet |  | |
| warfarin oral - | 4 mg tablet |  | |
| warfarin oral - | 2.5 mg tablet |  | |
| warfarin oral - | 7.5 mg tablet |  | |
| warfarin oral - | 10 mg tablet | 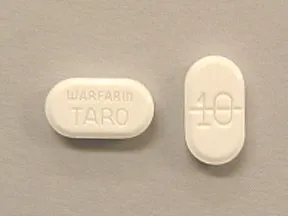 | |
| warfarin oral - | 7.5 mg tablet |  | |
| warfarin oral - | 6 mg tablet | 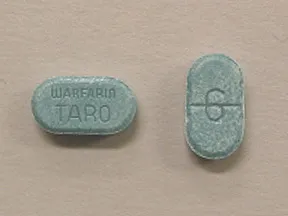 | |
| warfarin oral - | 1 mg tablet |  | |
| warfarin oral - | 3 mg tablet | 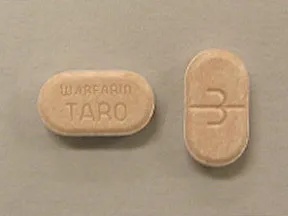 | |
| warfarin oral - | 2 mg tablet |  | |
| warfarin oral - | 4 mg tablet |  | |
| warfarin oral - | 2.5 mg tablet |  | |
| warfarin oral - | 2.5 mg tablet | 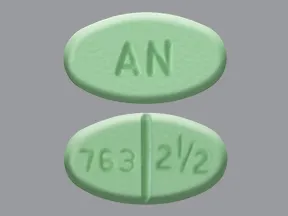 | |
| warfarin oral - | 10 mg tablet | 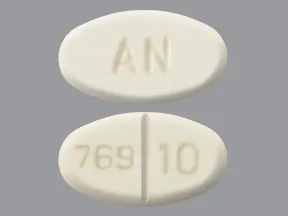 | |
| warfarin oral - | 7.5 mg tablet | 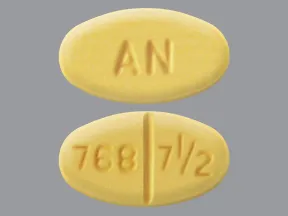 | |
| warfarin oral - | 7.5 mg tablet |  | |
| warfarin oral - | 10 mg tablet |  | |
| warfarin oral - | 1 mg tablet |  | |
| warfarin oral - | 6 mg tablet | 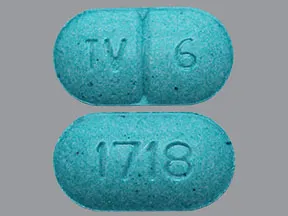 | |
| warfarin oral - | 3 mg tablet | 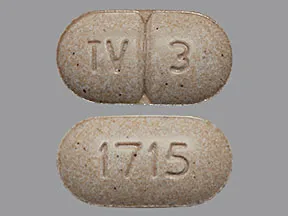 | |
| warfarin oral - | 7.5 mg tablet |  |
Copyright © 2010 First DataBank, Inc.
Patient Handout
warfarin oral
WARFARIN - ORAL
(WARF-uh-rin)
COMMON BRAND NAME(S): Coumadin, Jantoven
WARNING: Warfarin can cause very serious (possibly fatal) bleeding. This is more likely to occur when you first start taking this medication or if you take too much warfarin.To decrease your risk for bleeding, your doctor or other health care provider will monitor you closely and check your lab results (INR test) to make sure you are not taking too much warfarin. Keep all medical and lab appointments. Tell your doctor right away if you notice any signs of serious bleeding. See also Side Effects section.
USES: This medication is used to treat blood clots (such as in deep vein thrombosis-DVT or pulmonary embolus-PE) and/or to prevent new clots from forming in your body. Preventing harmful blood clots helps to reduce the risk of a stroke or heart attack. Conditions that increase your risk of developing blood clots include a certain type of irregular heart rhythm (atrial fibrillation), heart valve replacement, recent heart attack, and certain surgeries (such as hip/knee replacement).Warfarin is commonly called a "blood thinner," but the more correct term is "anticoagulant." It helps to keep blood flowing smoothly in your body by decreasing the amount of certain substances (clotting proteins) in your blood.
HOW TO USE: Read the Medication Guide provided by your pharmacist before you start taking warfarin and each time you get a refill. If you have any questions, ask your doctor or pharmacist.Take this medication by mouth with or without food as directed by your doctor or other health care professional, usually once a day. It is very important to take it exactly as directed. Do not increase the dose, take it more often, or stop using it unless directed by your doctor.The dosage is based on your medical condition, lab tests (such as INR), and response to treatment. Your doctor or other health care provider will monitor you closely while you are taking this medication to determine the right dose for you.Use this medication regularly to get the most benefit from it. To help you remember, take it at the same time each day.It is important to eat a balanced, consistent diet while taking warfarin. Some foods can affect how warfarin works in your body and may affect your treatment and dose. Avoid sudden large increases or decreases in your intake of foods high in vitamin K (such as broccoli, cauliflower, cabbage, brussels sprouts, kale, spinach, and other green leafy vegetables, liver, green tea, certain vitamin supplements). If you are trying to lose weight, check with your doctor before you try to go on a diet.Since this drug can be absorbed through the skin and lungs and may harm an unborn baby, women who are pregnant or who may become pregnant should not handle this medication or breathe the dust from the tablets.
SIDE EFFECTS: Nausea, loss of appetite, or stomach/abdominal pain may occur. If any of these effects last or get worse, tell your doctor or pharmacist promptly.Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.This medication can cause serious bleeding if it affects your blood clotting proteins too much (shown by unusually high INR lab results). Even if your doctor stops your medication, this risk of bleeding can continue for up to a week. Tell your doctor right away if you have any signs of serious bleeding, including: nosebleeds that happen often or don't stop, unusual pain/swelling/discomfort, unusual/easy bruising, prolonged bleeding from cuts or gums, unusually heavy/prolonged menstrual flow, pink/dark urine, coughing up blood, vomit that is bloody or looks like coffee grounds, severe headache, dizziness/fainting, unusual tiredness/weakness, bloody/black/tarry stools, chest pain, shortness of breath, difficulty swallowing.Tell your doctor right away if you have any serious side effects, including: nausea/vomiting that doesn't stop, severe stomach/abdominal pain, yellowing eyes/skin.This drug rarely has caused very serious (possibly fatal) problems if its effects lead to small blood clots (usually at the beginning of treatment). This can lead to severe skin/tissue damage that may require surgery or amputation if left untreated. Patients with certain blood conditions (protein C or S deficiency) may be at greater risk. Get medical help right away if any of these rare but serious side effects occur: painful/red/purplish patches on the skin (such as on the toe, breast, abdomen), signs of kidney problems (such as change in the amount of urine), vision changes, confusion, trouble speaking, weakness on one side of the body.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US -Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before taking warfarin, tell your doctor or pharmacist if you are allergic to it; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.Before using this medication, tell your doctor or pharmacist your medical history, especially of: blood disorders (such as anemia, hemophilia), bleeding problems (such as bleeding of the stomach/intestines, bleeding in the brain), blood vessel disorders (such as aneurysms), recent major injury/surgery, kidney disease, liver disease, alcohol use, mental/mood disorders (including memory problems), frequent falls/injuries.It is important that all your doctors and dentists know that you take warfarin. Before having surgery or any medical/dental procedures, tell your doctor or dentist that you are taking this medication and about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).Avoid getting injections into the muscles. If you must have an injection into a muscle (for example, a flu shot), it should be given in the arm. This way, it will be easier to check for bleeding and/or apply pressure bandages.This medication may cause stomach bleeding. Daily use of alcohol while using this medicine will increase your risk for stomach bleeding and may also affect how this medication works. Limit alcoholic beverages. Ask your doctor or pharmacist about how much alcohol you may safely drink.If you have not been eating well, if you have an illness or infection that causes fever, vomiting, or diarrhea for more than 2 days, or if you start using any antibiotic medications, contact your doctor or pharmacist right away because these conditions can affect how warfarin works.This medication can cause heavy bleeding. To lower the chance of getting cut, bruised, or injured, use great caution with sharp objects like safety razors and nail cutters. Use an electric razor when shaving and a soft toothbrush when brushing your teeth. Avoid activities such as contact sports. If you fall or injure yourself, especially if you hit your head, call your doctor right away. Your doctor may need to check you.The FDA has stated that generic warfarin products are interchangeable. However, consult your doctor or pharmacist before switching warfarin products. Be careful not to take more than one medication that contains warfarin unless specifically directed by the doctor or health care provider who is monitoring your warfarin treatment.Older adults may be at greater risk for bleeding while using this drug.Tell your doctor if you are pregnant or plan to become pregnant. You should not become pregnant while using warfarin. Warfarin may harm an unborn baby. Your doctor should order a pregnancy test before you start this medication. Ask about reliable forms of birth control while using this medication and for at least 1 month after the last dose. If you become pregnant, talk to your doctor right away about the risks and benefits of this medication. If you are planning pregnancy, discuss a plan for managing your condition with your doctor before you become pregnant. Your doctor may switch the type of medication you use during pregnancy.Since this drug can be absorbed through the skin and lungs and may harm an unborn baby, women who are pregnant or who may become pregnant should not handle this medication or breathe the dust from the tablets.Very small amounts of this medication may pass into breast milk but is unlikely to harm a nursing infant. Consult your doctor before breastfeeding.
DRUG INTERACTIONS: See also How to Use section.Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.Warfarin interacts with many prescription, nonprescription, vitamin, and herbal products. This includes medications that are applied to the skin or inside the vagina or rectum. The following interactions listed do not contain all possible drug interactions. The interactions with warfarin usually result in an increase or decrease in the "blood-thinning" (anticoagulant) effect. Your doctor or other health care professional should closely monitor you to prevent serious bleeding or clotting problems. While you are taking warfarin, it is very important to tell your doctor or pharmacist of any changes in medications, vitamins, or herbal products that you are taking.Some products that may interact with this drug include: imatinib, marijuana (cannabis), dronabinol, mifepristone, other drugs that can cause bleeding/bruising (including "blood thinners" such as apixaban/dabigatran).Aspirin, aspirin-like drugs (salicylates), and nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen, naproxen, celecoxib) may have effects similar to warfarin. These drugs may increase the risk of bleeding problems if taken during treatment with warfarin. Carefully check all prescription/nonprescription product labels (including drugs applied to the skin such as pain-relieving creams) since the products may contain NSAIDs or salicylates. Talk to your doctor about using a different medication (such as acetaminophen) to treat pain/fever. However, if your doctor has told you to take low-dose aspirin to prevent heart attack or stroke (usually 81-162 milligrams a day), you should keep taking the aspirin unless your doctor tells you not to. Ask your doctor or pharmacist for more details.This medication may interfere with certain lab tests (such as theophylline levels), possibly causing false test results. Make sure lab personnel and all your doctors know you use this drug.
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call 1-800-222-1222. Canada residents can call 1-844-764-7669. Symptoms of overdose may include: bloody/black/tarry stools, pink/dark urine, unusual/prolonged bleeding.
NOTES: Do not share this medication with others.Lab and/or medical tests (such as INR, complete blood count) must be done while you are taking this medication. Keep all medical and lab appointments. Consult your doctor for more details.
MISSED DOSE: For the best possible benefit, do not miss any doses. If you miss a dose, take it as soon as you remember. If you don't remember until the next day, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up because this could increase your risk for bleeding. Keep a record of missed doses to give to your doctor or pharmacist. Contact your doctor or pharmacist if you miss 2 or more doses in a row.
STORAGE: Store at room temperature away from light and moisture. Do not store in the bathroom. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
MEDICAL ALERT: Your condition can cause complications in a medical emergency. For information about enrolling in MedicAlert, call 1-888-633-4298 (US) or 1-800-668-1507 (Canada).
Information last revised May 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.







