By Darren Smith, Weekend Contributor
I found recently a video produced by the Parkinson’s Foundation that I believe offers both the general public and emergency responders an engaging primer toward accepting a beneficial mindset and foundation toward working with patients who experience hallucinations resulting from medication usage or have mental health issues.
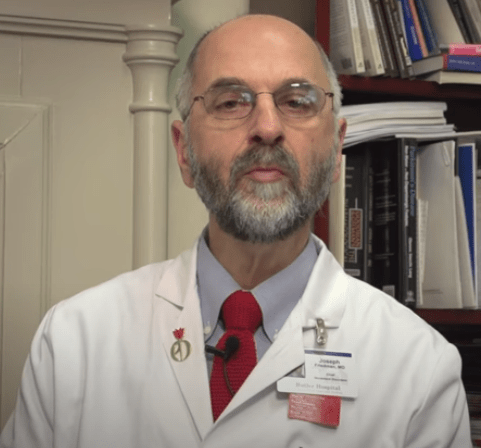
The below video was published on YouTube in 2018 by the Parkinson’s Foundation and narrated by Joseph H. Friedman, M.D. Director of the Movement Disorders Program at Butler Hospital and of the Department of Neurology, Alpert Medical School of Brown University. The presentation consists of Parkinson’s patients relating their experience with sensory hallucinations manifesting as the result of side-effects invoked via prescribed medication to treat their movement disorder. Dr. Friedman offers the viewer advice and insight as to why these experiences occur, which is of course valuable information, but in the larger scope of the human condition he provides a way for us to broaden our thinking and be more accepting of these conditions and relating to their challenges.
The basic tenet of this approach is to recognize in each of us that we have as a result of our upbringing, socialization, and at times own prejudices a predisposition in dealing with patients having hallucinations and manifestations of mental illnesses that can at worst be counterproductive or to a lesser degree evoke embarrassment or discomfort in the patient. But if instead we could better understand this process as being a condition or artifact of the process of perception, that it is not a failing or flaw in the character of the patient, we could then be more effective in relating to them.
The video shows only Parkinson’s patients who experience hallucinations but the approach can apply to those having mental illness.
I believe that at first glance in watching these patients’ descriptions it is easy to fall into the trap of dismissing their accounts as being bizarre, unfortunate, pitiful or otherwise but this is not a helpful mindset. A better strategy would be to cultivate in ourselves the acceptance that for these patients the combination of a neurodegenerative disease and the administration of medications to treat this disease can result in some changes to their perceptual process–That their interpretation of the world is modified as a result, and that it manifests in false interpretations by the mind. And like those of us not having these medical conditions, our interpretation of the world is also a consequence of our mind’s sensory perception. We might be interpreting these stimuli correctly and they at times might not be. It is not a failing of this person’s character or value as a person.
When these patients are having a hallucination or delusion, it is important to recognize that for them their perceived reality is just as valid and true is it might be for those of us not afflicted. Resultant from this, the mind tries to form an interpretation of these false perceptions and based upon this “evidence”, as it might be called, the patient’s behavior reacts to this perceived reality accordingly. In some anecdotes I will later illustrate how their actions might be reasonable based upon their own view of the world, thought it isn’t necessarily for others’.
One helpful technique I found for myself in developing a working relationship with such patients is to look with interest on how their individual hallucination or behavior presents itself. Some have been very interesting in their intricacy and difference from what I would see in the world. And there have been occasions where I pondered how the human mind can arrive at such thoughts. It seemed that after taking this approach, it became almost automatic that I could bypass the judgmental reactions and take a general interest in this person, as they were a source of interest. Their experiences does offer in some ways an alternative way of trying to understand the human mind and how it formulates thought and what it considers important or significant. When we find others to be interesting we are less likely to be condescending or critical. And people do pick up with great acuity when others are thinking negatively of them, especially when trying to hide it. The patients are often very sensitive to being judged. If we can ourselves get past being critical we can gain their trust and have a more engaging and useful experience with others.
Another strategy is to change how we define hallucinations and such. For many, the term “hallucination” carries with it connotations of illness, misbehavior, inability, or perhaps even malice. A more helpful method would be to view these manifestations as Artifacts. (In human sensory perception).
While not trying to be dismissive as to the human condition of having to experience these artifacts, if one does accept these artifacts as simply a misinterpretation of sensory input or as a result of a process of formulating an image we remove the emotion and pretense. We can see in other situations an analogue between the human mind and in the below case of a digital camera interpreting an image based on the lens’ direction of light that is then processed by the camera’s electronics.
Of course we know that when this image was taken, there were no large colored disks adjoining a waterfall. Yet nevertheless these two artifacts present themselves to the viewer in the field of vision just the same as the other surroundings. Most of us recognize that these disks are not real in the actual sense because we have learned during our lives that these manifestations are products of the photographic process that sometimes occur during certain conditions. As casual photographers, we use our experience to avoid such conditions as they often detract from what we view as good picture taking. But in the case of someone experiencing challenges with hallucinations and such, it can be difficult to distinguish between what is actual and what is resultant from a false sensory perception, especially when these take on compelling levels of nuance and mirror that of reality. Another example, this time of a false perception artifact, is this example relating to Migraine Headaches or Epilepsy:
The above is an artist’s rendition of what they have personally experienced. Again, it is a false perception resulting from neurochemical processes. It is not in any manner a measure of quality of this person or their ability to live successfully in the world. It is simply an effect of certain conditions unique to this individual.
The degree of variance between presentations of hallucinations or illness is as vast as the realm of human thought. And the degree of interference these conditions cause in a person’s life is as such and by extension applies consequently to those around them.
Two cases come to mind that demonstrate how a person’s misperception of sensory input and thinking can elicit behavior that is for them “reasonable” but might not seem that way for others.
The first was a patient, afflicted with schizophrenia, experienced strongly convincing delusions of threats from others. In their case it manifested in the mistaken belief that “…people were coming out of mirrors.” In this incident the family called because the afflicted family member was smashing all the mirrors in the house and could not be calmed or discouraged form breaking things. The patient stated that the “people” were trying to hurt their family members and to prevent them from burglarizing the house he smashed the mirrors to thwart their entry.
Now from a law enforcement perspective what do you do if called to this situation? Some rather hard-lined thinkers might simply declare that this was an act of malicious mischief and levy a criminal sanction against the patient. But is there an affirmative defense to this person’s actions–that of self-defense? I believe there is a credible argument to support such a suggestion.
Much of the criminal law or defenses to such import the notion of what a “reasonable person” would do in the same situation. Certainly breaking mirrors to prevent hallucinations of persons from passing through them is not a reasonable proposition. But when we couple that with a common adjunct to the idea of the “reasonable person”–the information\evidence available at the time of the event to that person–the defense is often provable. If ordinary persons in their homes saw that strangers were trying to shove their way past the door it is unquestionably reasonable for the homeowner to fight back and close the door to prevent intruders from entering the household. We interpret via our senses the threat of someone breaking in and we act accordingly. Yet in the case of this patient, due to his then currently manifesting perceptual errors, artifacts in his thinking presented him with compelling, though false, evidence that he and his family were being threatened by those entering the house and he took what he considered to be reasonably necessary steps to protect everyone. Should we arrest this patient or praise him for saving his home from invaders? I believe this patient’s actions did not constitute a criminal liability. It was the result of false perceptions form a person having an illness: something that is just an unfortunate part of the human experience.
In the second example we have a patient who has the belief that she transitions into a form of vampire when certain conditions are met. I remember seeing her on one occasion where she went out to check her mail covering herself nearly completely within a blanket. It was not cold outside nor was it raining. Why was she doing this? I later realized that she had entered her vampire state and, at least according to the legend, she would be vulnerable to the hazardous effects of sunlight. She needed to get her mail, and under the false assumption she was a vampire, the safest thing she could do was to cover up when in the sunlight. It was to her as ordinary and reasonable as police officers putting on body armor when getting ready for work to protect themselves from being shot or an electrical contractor donning Personal Protective Equipment to prevent them from being burned when servicing high voltage transformers. The underlying perceptions were falsehoods but these two persons were acting accordingly and to them rationally based on that information. It is paramount in dealing with these individuals that we accept that their own form of reality is just as valid and legitimate to them as ours is to us.
My experiences with those having these challenges are that the outcome of a situation involving them is highly dependent on how we present ourselves. One important strategy, and there are many others of course, is to accept that we are eventually going to need to deal with a person having health issues such as these and to prepare ourselves to accept their individual condition as being a medical manifestation and that this person is just as important and equal as we are in our own realm. Statistically speaking, it was really just a matter of rolling the dice in terms of genetics, events, or circumstance that made us who we are and it was often just chance and statistics that might bring you or I to later have a similar medical condition sometime in the future. And if it does happen to us, we are not demoted or diminished either. It’s just a medical process that might happen to us as well. So who are we to judge these patients today?
From there it is often beneficial to the situation to talk to the patient as if we were conversing with one of your own peers about something ordinary and non-controversial. It is important not to “talk down” to this person, patronize them, or be dismissive. Think of how you would feel if you said that you believed the sunset to be warm and spiritual only to be shot down as being stupid or crazy for suggesting such a thing. Now imagine having to live with a health condition that evokes rebuke from others on a daily basis, for years and years unrelentingly. What would that do to your happiness or your willingness to relate to others? Imagine that instead perhaps for the first time in this patient’s week someone (you) actually spoke to them in an adult manner and worked with them in a matter-of-fact way to alleviate what might be upsetting to them. Then if you are in a position where you are charged with attending to this person’s immediate needs, you can do so effectively and in a manner they find agreeable.
Returning to Dr. Friedman’s presentation, I strongly recommend learning and taking to heart the manner and demeanor in which he details the Parkinson’s patients’ conditions. Adapting your personal approach to mental health patients to mirror how Dr. Friedman applies his profession will afford you a good basis for which to relate to these patients and accept who they are and their health condition.
By Darren Smith
Photo Credit (Aura): Tehom
The views expressed in this posting are the author’s alone and not those of the blog, the host, or other weekend bloggers. As an open forum, weekend bloggers post independently without pre-approval or review. Content and any displays or art are solely their decision and responsibility.

