PART TWO: CONNECTIVE TISSUE AND HYPERMOBILITY SPECTRUM DISORDERS
3.0 An Overview of Connective Tissue
The human body consists of four types of tissue:
- Epithelial Tissue:
a. This tissue type covers body surfaces and lines body cavities providing protection and allowing for the absorption and secretion of substances. - Muscle Tissue:
a. Excitable cells capable of contraction allow muscle tissue to generate body movement. - Nervous Tissue:
a. This primary tissue of the nervous system allows for communication between various organs and tissues.
b. It is composed of neurons and glial cells. - Connective Tissue:
a. Outlined in this part of the article.
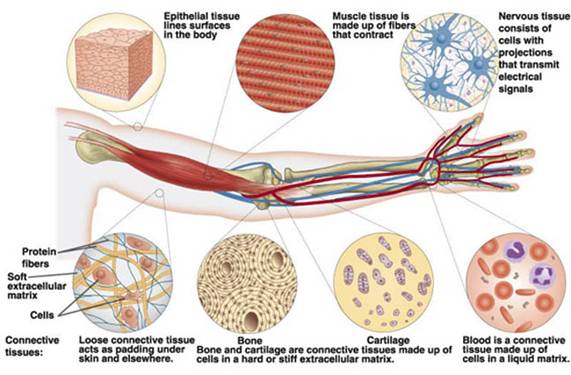
3.1 The Purpose of Connective Tissue
The purpose of connective tissue is, obviously, to connect. It achieves this function by supporting and binding other tissues in the body, however, unlike epithelial tissue – which has cells that are closely packed together – connective tissue typically has cells scattered throughout an extracellular matrix of fibrous proteins and glycoproteins attached to a basement membrane.
In short, connective tissue is incredibly diverse and contributes to energy storage, the protection of organs, the body’s structural integrity. Therefore its major functions include:
- Binding and supporting;
- Protecting;
- Insulating;
- Storing reserve fuel; and
- Transporting substances within the body.
It is important to note that connective tissues can have various levels of vascularity, for example:
- Cartilage is avascular (i.e. few or no blood vessels);
- Dense connective tissue (discussed below) is poorly vascularised; and
- Others, such as bone, are richly supplied with blood vessels.
Further, over 100 different connective tissue disorders have been described (Faghfoury, 2014).

3.2 Elements of Connective Tissue
The primary elements of connective tissue include:
- A ground substance: The ground substance acts as a fluid matrix that suspends the cells and fibres within the particular connective tissue type.
- Fibres and cells: Connective tissue fibres and matrix are synthesised by specialised cells called fibroblasts.
3.3 Types of Connective Tissue
There are three main groups of connective tissues:
- Loose Connective Tissue:
- In vertebrates, the most common type of connective tissue is loose connective tissue.
- It holds organs in place and attaches epithelial tissue to other underlying tissues.
- Loose connective tissue is named so because of the ‘weave’ and type of its constituent fibres.
- These fibres form an irregular network with spaces between the fibres.
- The spaces are filled with ground substance.
- The three main types of loose connective fibres include:
- Collagenous fibres are made of collagen and consist of bundles of fibrils that are coils of collagen molecules. These fibres help to strengthen connective tissue.
- Elastic fibres are made of the protein elastin and are stretchable. They help to give connective tissue elasticity.
- Reticular fibres join connective tissues to other tissues.
- Loose connective tissues provide support, flexibility, and strength required to support internal organs and structures such as blood vessels, lymph vessels, and nerves.
- Dense Connective Tissue:
- Another type of connective tissue is dense or fibrous connective tissue, which can be found in tendons and ligaments.
- These structures help attach muscles to bones and link bones together at joints.
- Dense connective tissue is composed of large amounts of closely packed collagenous fibres.
- In comparison to loose connective tissue, dense tissue has a higher proportion of collagenous fibres to ground substance.
- It is thicker and stronger than loose connective tissue and forms a protective capsule layer around organs such as the liver and kidneys.
- Dense connective tissue can be categorised into dense regular, dense irregular, and elastic connective tissues:
- Dense regular: Tendons and ligaments are examples of dense regular connective tissue.
- Dense irregular: Much of the dermis layer of the skin is composed of dense irregular connective tissue. The membrane capsule surrounding several organs is also dense irregular tissue.
- Elastic: These tissues enable stretching in structures such as arteries, vocal cords, the trachea, and bronchial tubes in the lungs.
- Soft Connective Tissue:
- Some sources combine loose and dense into one group known as:
- Soft connective tissue; or
- Connective tissue proper.
- Some sources combine loose and dense into one group known as:
- Specialised Connective Tissue:
- Specialised connective tissues include a number of different tissues with specialised cells and unique ground substances.
- Some of these tissues are solid and strong, while others are fluid and flexible.
- Examples include:
- Adipose Tissue:
- Adipose tissue is a form of loose connective tissue that stores fat.
- Adipose lines organs and body cavities to protect organs and insulate the body against heat loss.
- Adipose tissue also produces endocrine hormones that influence activities such as blood clotting, insulin sensitivity, and fat storage.
- The primary cells of adipose are adipocytes.
- These cells store fat in the form of triglycerides.
- Adipocytes appear round and swollen when fat is being stored and shrink as fat is used.
- Most adipose tissue is described as white adipose which functions in the storage of energy.
- Both brown and beige/brite adipose burn fat and produce heat (Giralt & Villarroya, 2013).
- Cartilage:
- Cartilage is a form of fibrous connective tissue that is composed of closely packed collagenous fibres in a rubbery gelatinous substance called chondrin.
- The skeletons of sharks and human embryos are composed of cartilage.
- Cartilage also provides flexible support for certain structures in adult humans including the nose, trachea, and ears.
- There are three different types of cartilage, each with different characteristics.
- Hyaline cartilage is the most common type and is found in areas such as the trachea, ribs, and nose. Hyaline cartilage is flexible, elastic, and surrounded by a dense membrane called perichondrium.
- Fibrocartilage is the strongest type of cartilage and composed of hyaline and dense collagen fibres. It is inflexible, tough, and located in areas such as between vertebrae, in some joints, and in heart valves. Fibrocartilage does not have perichondrium.
- Elastic cartilage contains elastic fibres and is the most flexible type of cartilage. It is found in locations such as the ear and larynx (voice box).
- Bone Tissue:
- Bone is a type of mineralised connective tissue that contains collagen and calcium phosphate, a mineral crystal.
- Calcium phosphate gives bone its firmness.
- There are two types of bone tissue:
- Spongy bone, also called cancellous bone, gets its name because of its spongy appearance. The large spaces, or vascular cavities, in this type of bone tissue contain blood vessels and bone marrow. Spongy bone is the first bone type formed during bone formation and is surrounded by compact bone.
- Compact bone, or cortical bone, is strong, dense, and forms the hard outer bone surface. Small canals within the tissue allow for the passage of blood vessels and nerves. Mature bone cells, or osteocytes, are found in compact bone.
- Blood and Lymph:
- Interestingly enough, blood is considered to be a type of connective tissue.
- Like other connective tissue types, blood is derived from mesoderm, the middle germ layer of developing embryos.
- Blood also serves to connect other organ systems together by supplying them with nutrients and transporting signal molecules between cells.
- Plasma is the extracellular matrix of blood with red blood cells, white blood cells, and platelets suspended in the plasma.
- Lymph is another type of fluid connective tissue.
- This clear fluid originates from blood plasma that exits blood vessels at capillary beds.
- A component of the lymphatic system, lymph contains immune system cells that protect the body against pathogens.
- Lymph is delivered back to blood circulation via lymphatic vessels.
3.4 Linking Ligaments, Tendons, Muscles and Bones
It is also important to note the role of ligaments, tendons, muscles, and bones. Simply put, ligaments connect bone to bone and tendons connect muscle to bone.
In healthy connective tissue muscle can be likened to a rubber band whilst a tendon is likened to a metal coil. In EDS and HSD, the tendon is the rubber band and the muscle is the metal coil, and ligaments, which should be as tight as a metal coil, are more like a rubber band.
3.5 Types of Collagen
Collagen is the major insoluble fibrous protein in the extracellular matrix and in connective tissue.
“In fact, it is the single most abundant protein in the animal kingdom.” (Lodish et al., 2000).
Collagen is the building block for many parts of the body, including skin (about 70%-75% of the dry weight of your skin), bones, and tendons. It can also be found in our hair, joints, eyelashes, nails, muscles in general, teeth, and even our stomach lining. Collagen is also rich in amino acids which you need to maintain and repair your tendons, bones, and joints. As we get older, we break collagen down faster than we can replace it.
There are at least 16 types of collagen, but 80% to 90% of the collagen in the body consists of types I, II, and III. These collagen molecules pack together to form long thin fibrils of similar structure. In contrast, Type IV, forms a two-dimensional reticulum; several other types associate with fibril-type collagens, linking them to each other or to other matrix components. Types I, II, III, and V are considered fibrillar collagens, types VI and IX are considered fibril-associated collagens, and type IV is considered a sheet-forming collagen (Lodish, 2000).

There are 18 amino acids in collagen, including:
- Glycine (an essential amino acid) is important in blocking endotoxin (a compound that activates inflammatory signals and can lead to low thyroid levels).
- Proline (an essential amino acid) is important for the stimulation of collagen synthesis as well as acting as an antioxidant and preventing cell damage from free radicals.
- Glutamine helps prevent gut inflammation.
- Arginine which may be able to help synthesise creatine for increased athletic performance.
Previously it was thought that all collagens were secreted by fibroblasts in connective tissue, but it is now known that numerous epithelial cells make certain types of collagens.
The various collagens and the structures they form all serve the same purpose, to help tissues withstand stretching.
4.0 An Overview of Hypermobility Spectrum Disorders
Hypermobility spectrum disorders (HSD) are a group of conditions related to joint hypermobility. HSD are usually limited to muscles, joints, and bones (Castori et al., 2017).
HSD are intended to be diagnosed after all other possible conditions are excluded, such as any of the EDS, including hEDS. The 2017 hEDS criteria established serious consideration of joint hypermobility with all related symptoms and conditions, with hEDS at one end of the spectrum.
Similar to hEDS, HSD can have significant effects on an individual’s health and can be equal in severity – and both require similar management, validation, and care. HSD range from joint hypermobility with no other symptoms to complex HSD that can have the same life-altering symptoms as hEDS.
The essential difference between HSD and hEDS lies in the stricter criteria for hEDS compared to the HSD, and reflects the more likely hereditary and/or systemic nature of hEDS compared to HSD. The term HSD relates, in fact, to a wide range of musculoskeletal manifestations that can be considered “secondary to” the underlying joint hypermobility.
Treatment for HSD symptoms is the same as treatment for hEDS.
4.1 Types of Joint Hypermobility
Joint hypermobility (JH) is the term used to describe the capability of joints to move beyond normal limits – it is a descriptor rather than a diagnosis – and can exist by itself or as part of a more complex diagnosis.
JH is also known as (Tinkle et al., 2017):
- Joint hypermobility syndrome (JHS);
- Hypermobility syndrome; and
- Benign joint hypermobility syndrome.

Types of joint hypermobility include:
- Localised joint hypermobility (LJH):
- JH in one to four joints.
- Generalised joint hypermobility (GJH):
- JH in five or more joints.
- Possibly inherited.
- Acquired forms exist including:
- Training, such as dance;
- Inflammatory or degenerative diseases; and
- Hyperthyroidism and other endocrine disorders.
- Occurs in approximately 2-57% of different populations (3.3% females and 0.6% males); this may be due to the use of different assessment methods and criteria for classification (Section 4.4 below).
- Peripheral joint hypermobility (PJH):
- Affects the hands and/or feet only.
- Common in infants, toddlers, and children, in whom it is usually mild or has no serious effect.
- Distinguished from GJH by the absence of large joint involvement.
- Historical joint hypermobility (HJH):
- Found in older adults who have progressively lost JH.
- Joints can become more rigid with age.
In 2017, Castori et al (2017) proposed classifying JH as:
- Individuals with LJH, PJH, or GJH without symptoms.
- Individuals with a well-defined disorder with JH, also comprising hEDS.
- Individuals with symptoms associated with JH but not satisfying the criteria/diagnosis for a syndrome. For these individuals the term HSD was proposed.
It is important to note that JH may occur without symptoms in multiple individuals from the same family, with or without hEDS occurring in that family (Castori et al., 2017).
4.2 Joint Instability
Joint instability (JI) has in the past been used as a synonym of JH. However, JI indicates the pathological process manifesting with recurring damage, while JH is a broader condition of excessive movement of the joint. Therefore, JI can be considered a possible complication of JH, which, in turn, does not show symptoms. Not all unstable joints are hypermobile.
4.3 Types of Hypermobility Spectrum Disorder
Table 3 outlines the types of HSD.
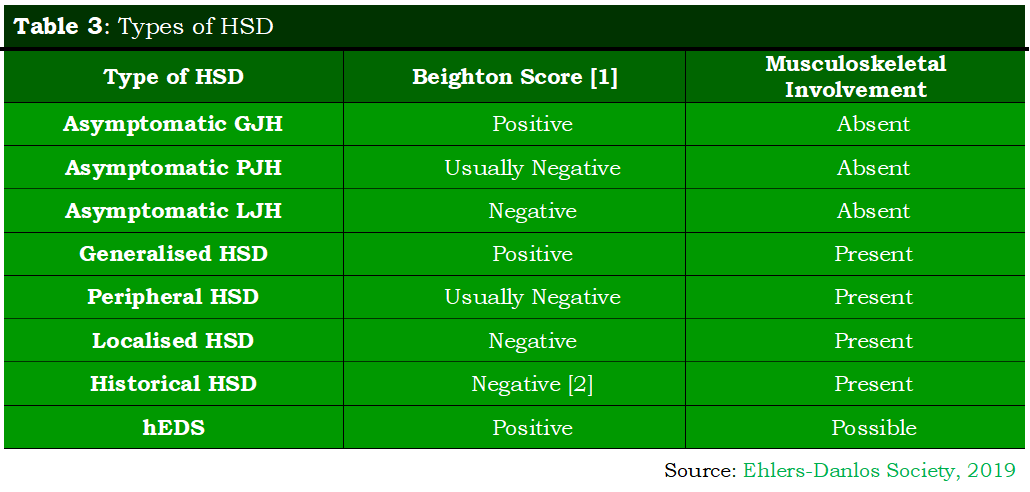
Notes:
- For detail on the Beighton Score refer to Section 4.4.
- Historical presence of JH (e.g. positive 5-point questionnaire).
4.4 Assessment Methods for Classifying GJH
There are a number of assessment methods for classifying GJH (including but not limited to) (Juul-Kristensen et al., 2017):
- Clinical:
- Beighton Score (BS);
- Carter and Wilkinson (CW);
- Hospital del Mar (HdM); and
- Rotes-Querol (RQ).
- Questionnaire:
- Five-part questionnaire (5PQ), aka the hypermobility questionnaire; and
- Beighton Score-self reported (BS-self).
The Beighton Score, a modification of the Carter and Wilkinson scoring system, is a set of manoeuvres used to judge if there is evidence of joint hypermobility (Beighton et al., 1973), and consists of:
- One point if, while standing and bending forward, the individual can place their palms on the ground with the legs straight.
- One point for each elbow that extends more than 10 degrees.
- One point for each knee that extends more than 5 degrees.
- One point for each thumb that, with the wrist flexed, can be manipulated to the forearm.
- One point for each fifth finger that extends beyond 90 degrees.
There are 9 points, and a score of 4 or more is considered a sign that GJH is present.
The Beighton score is best used as a screening tool and, thereafter, other sites should be examined for hypermobility, including the temporomandibular joint, cervical spine, shoulders, thoracic spine, hips, ankles, and feet.
For the purposes of diagnosing hEDS, GJH is confirmed by a score of (out of 9) (Malfait et al., 2017):
- ≥6 for pre-pubertal children;
- ≥5 for pubertal children and adults up to age 50; and
- ≥4 for those age >50 years.
It is important to note that multiple other variables including (but not limited to) ethnicity, gender, trauma, surgery, arthritic change, conditioning, and stretching also affect the Beighton score.
Allied to the Beighton score is the 5PQ, so far only used for adults, which can be used instead of a physical examination (Hakim & Grahame, 2003). The five questions are:
- Can you now (or could you ever) place your hands flat on the floor without bending your knees?
- Can you now (or could you ever) bend your thumb to touch your forearm?
- As a child did you amuse your friends by contorting your body into strange shapes OR could you do the splits?
- As a child or teenager did your shoulder or kneecap dislocate on more than one occasion?
- Do you consider yourself double-jointed?

An answer of ‘yes’ to two or more of the questions gives a very high prediction of the presence of hypermobility, with 85% sensitivity and specificity against the Beighton Score.
Points to note:
- GJH may be confirmed in an individual whose Beighton Score is one point below the age-specific cut-off if there are two or more positive answers to the 5PQ (Hakim & Grahame, 2003).
- Individuals with prior history of joint hypermobility, suggested by a positive 5PQ (≥2 positive answers) but scoring two or more points below the age specific Beighton cut-off, should not be considered to have GJH and should instead be evaluated for HSD (Castori et al., 2017).
4.5 Problems Associated with Joint Hypermobility
Although joint hypermobility can be symptomless, apart from the unusual mobility, there is a series of other symptoms that result from that mobility (known as secondary musculoskeletal manifestations):
- Trauma:
- Macrotrauma includes dislocation, subluxations, and connected soft tissue damage (ligaments, tendons, muscles). It can cause acute pain and loss of joint function.
- Microtrauma are injuries too small for them to be noticed as they happen. Over time, they may make one susceptible to recurrent or persistent pain, and possibly early joint degeneration like osteoarthritis.
- Chronic Pain:
- Occasional, recurring pain is a natural result of the trauma, but chronic pain can develop – perhaps because of:
- Hyperalgesia (unusual sensitivity to pain); or
- An impaired connective tissue function (as suggested by the discovery of small fibre neuropathy in adults with classical, hypermobile, and vascular EDS).
- Occasional, recurring pain is a natural result of the trauma, but chronic pain can develop – perhaps because of:
- Disturbed Proprioception:
- Proprioception is the sense of the relative position of parts of the body.
- Disturbed proprioceptive information can induce illusions of distorted body perception.
- This can include:
- Suboptimal postural orientation;
- Decreased stability; and/or
- Dizziness.
Other associated problems not based in the musculoskeletal system (i.e. not the direct result of the mechanics of JH) include:
- Anxiety disorders.
- Orthostatic tachycardia:
- Postural orthostatic tachycardia syndrome (POTS) is a condition in which a change from lying to standing causes an abnormally large increase in heart rate. Diagnosis in adults is based on an increase in heart rate of more than 30 beats per minute within ten minutes of standing up which is accompanied by symptoms.
- POTS affects many different people, but is most common in girls and women aged 15 to 50.
- Variety of functional gastrointestinal disorders.
- Pelvic and bladder dysfunction.
Other inherited disorders of the soft connective tissue with JH include Marfan syndrome. People with Marfan tend to be tall and thin, with long arms, legs, fingers and toes. They also typically have flexible joints and scoliosis.
| Back to Part One | Continue to Part Three |


You must be logged in to post a comment.