This edition of Coding Quarterly highlights appropriate coding for oximetry to capture both practice expense and physician work as well as review of evaluation and management (E/M) coding.
Coding scenario
Mr. Smith, an established patient, was recently diagnosed with severe sleep apnea by a home sleep apnea test and has been on APAP for one month. He lives two hours outside of Sheridan, WY (elevation 3,743 ft), has obesity (BMI 33), hypertension, hyperlipidemia, asthma, diabetes, post-traumatic stress disorder and hemoglobin of 17.9 g/dl. Review of his PAP data at one month shows excellent adherence and efficacy of the device in treating his sleep apnea. His baseline study oxygen parameters showed an oxygen desaturation index (ODI) of 82/h, average SpO2 of 92.3%, minimum saturation 77%, SpO2 duration less than 90% of 74%, SpO2 duration less than or equal to 88% of 56%, and SpO2 duration less than 85% of 17%. Given his excellent PAP use, nocturnal oximetry is ordered to evaluate whether his significantly reduced oxygenation on baseline study has resolved with PAP therapy. He completes overnight oximetry on PAP, and oxygenation data is compared to the same night data from his PAP device. ODI is 3.5/h, average SpO2 is 93.6%, minimum saturation is 86%, SpO2 duration less than 90% of 5.7%, SpO2 duration less than or equal to 88% of 1.3%, SpO2 duration less than 85% of 0%. Time spent reviewing oximetry data and comparing it to detailed flow from PAP device, contacting the patient to notify him of results, and charting his results and medical recommendations that supplemental oxygen is not indicated was 22 minutes. By doing overnight oximetry, an in-laboratory efficacy study was not needed, which reduced travel burden for this patient.
Coding recommendation
If you want to capture physician work and time, you could bill an appropriate E/M code in addition to 94762 (noninvasive ear or pulse oximetry for oxygen saturation, by continuous overnight monitoring). 94762 is a practice expense only code and does not include physician work. The choice of E/M code will depend on the specific circumstances of the encounter, including the level of complexity of the patient’s condition and the intricacy of medical decision making (MDM).
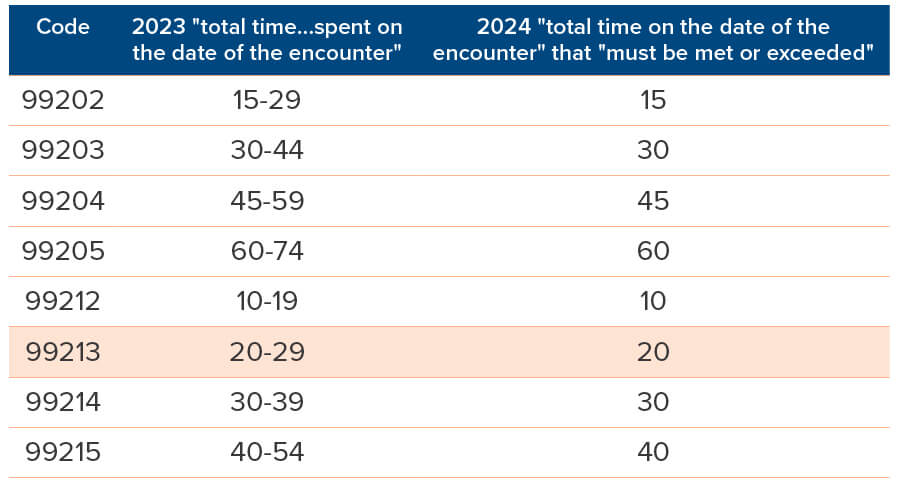
Based upon AMA CPT Guidelines for E/M coding for total time of 22 minutes, the appropriate level of E/M service to bill for this encounter is 99213 with modifier 25, along with 94762.
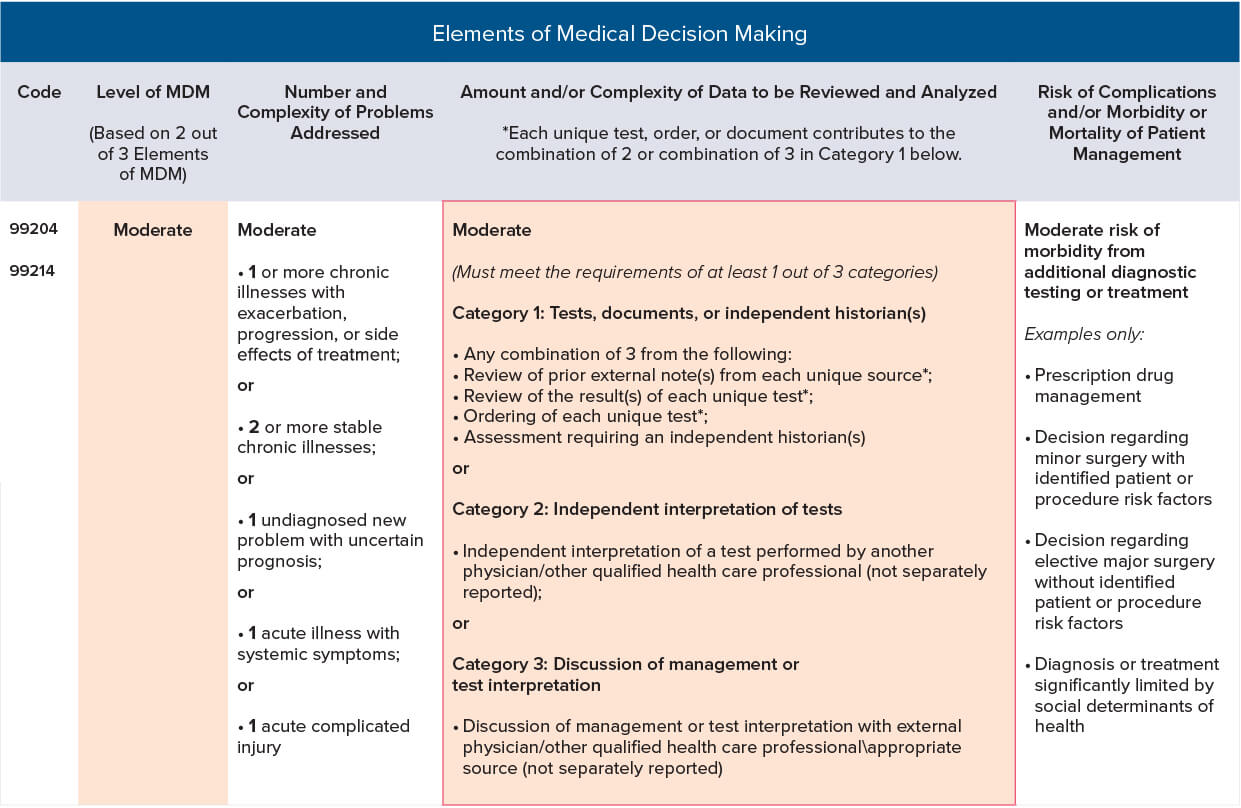
Based on the notes, the appropriate level of E/M service can be determined using the MDM component. MDM considers the complexity of establishing a diagnosis and managing the patient’s condition. In this case, the complexity of the patient’s medical problems, the need for data review, and the MDM involved suggest a moderate level of MDM.
Let’s break down the MDM elements:
- Number of diagnoses or management options: The patient has multiple chronic conditions including severe sleep apnea, obesity, hypertension, hyperlipidemia, asthma, diabetes, PTSD and elevated hemoglobin. Additionally, there is the need to evaluate oxygenation parameters. This indicates a moderate number of diagnoses or management options.
- Amount and/or complexity of data to be reviewed: The provider reviewed data from the patient’s PAP device, including oximetry data, and compared it to baseline study results. This involves reviewing and interpreting multiple data points, indicating a moderate level of complexity.
- Risk of complications and/or morbidity or mortality: The patient has several chronic conditions, including severe sleep apnea and obesity, which can lead to significant complications if not managed properly. However, the provided notes do not specify any acute exacerbation or imminent risk factors. Therefore, the risk level can be considered low.
Based on the above assessment, the MDM complexity level would be moderate. According to the 2021 E/M documentation guidelines, a moderate complexity MDM warrants a level 4 E/M service.
Therefore, the appropriate level of E/M service to bill for this encounter using MDM would be 99214 with modifier 25, along with 94762. (See the following table for additional details about the elements of MDM.)
(When billing E/M services, coding is based upon either MDM or total time spent on the same day of the encounter. Total time includes both time with a patient and any pre- or post-work; document the exact number of minutes, not the range.)
The methodology that accounts for the most appropriate and relevant elements for a given patient visit should be used to select the appropriate level of E/M. As an example, a high-intensity E/M that lasts a brief period might be more appropriately reflected using MDM. A time-sensitive visit might be better captured using time as the criteria for the level of E/M.
Coding Pro Tips
- Be sure to document the medical necessity and the distinct services provided when billing multiple codes for a single encounter.
- Be aware of any payer-specific coding guidelines or bundling rules that may affect reimbursement.
Members may send coding questions and use cases they would like to have featured in the Coding Quarterly to coding@aasm.org.
About AASM Coding Quarterly
The AASM Coding Quarterly is developed by the Coding and Reimbursement Advisory Committee to explain complicated coding scenarios and provide recommendations for correct coding using current procedural terminology (CPT) and ICD-10-CM codes. The AASM recommends that all members also review payer policies, as coding and documentation requirements vary by payer.
Tables are adapted from the AMA Current Procedural Terminology. CPT is a registered trademark of the American Medical Association. Copyright 2021 AMA. All rights reserved.





