Dosing & Uses
Dosage Forms & Strengths
tablet
- 100mg
- 150mg
Ovarian Cancer
Recurrent ovarian cancer
- Indicated as maintenance treatment for recurrent ovarian cancer (including epithelial ovarian, fallopian tube or primary peritoneal cancer) in adults who are in complete or partial response to platinum-based chemotherapy
- 300 mg PO BID
- Continue until disease progression, unacceptable toxicity
Advanced ovarian cancer (monotherapy)
- Indicated as first-line maintenance treatment for deleterious or suspected deleterious somatic or germline BRCA-mutated (gBRCAm) advanced ovarian cancer in patients who are in complete or partial response to first-line platinum-based chemotherapy
- 300 mg PO BID
- Continue until disease progression, unacceptable toxicity, or completion of 2 years of treatment
-
Completion of 2 years of treatment
- Patients with complete response (no radiologic evidence): Stop treatment
- Patients with evidence of disease and may benefit from continuous treatment: Treat beyond 2 years
Advanced ovarian cancer (combination therapy)
- Indicated as first-line maintenance treatment for advanced ovarian cancer in combination with bevacizumab for adults who are in complete or partial response to first-line platinum-based chemotherapy and whose cancer is associated with homologous recombination deficiency (HRD) positive status defined by either a deleterious or suspected deleterious BRCA mutation, and/or genomic instability
- Olaparib 300 mg PO BID, plus
- Bevacizumab 15 mg/kg IV q3Weeks for a total of 15 months (including with chemotherapy and as maintenance)
- Continue until disease progression, unacceptable toxicity, or completion of 2 years of treatment
- Refer to prescribing information for bevacizumab when used in combination with olaparib for more information
-
Completion of 2 years of treatment
- Patients with complete response (no radiologic evidence): Stop treatment
- Patients with evidence of disease and may benefit from continuous treatment: Treat beyond 2 years
Advanced ovarian cancer (after ≥3 lines of chemotherapy)
- Indication was voluntarily withdrawn in the U.S. by manufacturer on August 26, 2022
- The decision was made in consultation with the FDA after the final overall survival analysis indicated a potential detrimental effect on overall survival for the olaparib-treated arm compared to the control arm in patients who received 3 or more prior lines of chemotherapy in the Phase III SOLO3 study
- Do not initiate olaparib for deleterious or suspected deleterious gBRCAm advanced ovarian cancer in adults previously treated with 3 or more lines of chemotherapy
- Consult and share information with patients currently treated for such indication so they may make an informed decision regarding their ongoing care
Breast Cancer
High-risk early breast cancer
- Indicated for adjuvant treatment of deleterious or suspected deleterious gBRCAm human epidermal growth factor receptor 2 (HER2)-negative high-risk early breast cancer in adults previously treated with neoadjuvant or adjuvant chemotherapy
- 300 mg PO BID
- Continue for a total of 1 year, or until disease recurrence, or unacceptable toxicity, whichever occurs first
- Patients receiving olaparib for hormone receptor positive HER2-negative breast cancer should continue concurrent treatment with endocrine therapy as per current clinical practice guidelines
Metastatic breast cancer
- Indicated for deleterious or suspected deleterious gBRCAm, HER2-negative metastatic breast cancer
- Patients who have been treated with chemotherapy in the neoadjuvant, adjuvant, or metastatic setting
- Patients with hormone receptor (HR)-positive breast cancer should have been treated with prior endocrine therapy or be considered inappropriate for endocrine therapy
- 300 mg PO BID
- Continue treatment until disease progression or unacceptable toxicity
Pancreatic Cancer
Indicated for first-line maintenance treatment of adults with deleterious or suspected deleterious gBRCAm metastatic pancreatic adenocarcinoma whose disease has not progressed on at least 16 weeks of a first-line platinum-based chemotherapy regimen
300 mg PO BID
Continue treatment until disease progression or unacceptable toxicity
Metastatic Castration-Resistant Prostate Cancer
Homologous recombination repair (HRR) gene-mutated metastatic castration-resistant prostate cancer (mCRPC)
- Indicated for deleterious or suspected deleterious germline or somatic HRR gene-mutated mCRPC in adults who have progressed following prior treatment with enzalutamide or abiraterone
- 300 mg PO BID
- Continue until disease progression or unacceptable toxicity
- Should also receive a gonadotropin-releasing hormone (GnRH) analog concurrently or should have had bilateral orchiectomy
BRCA-mutated mCRPC
- Indicated in combination with abiraterone and prednisone or prednisolone, for deleterious or suspected deleterious BRCA-mutated mCRPC
- 300 mg PO BID, PLUS
- Abiraterone 1000 mg PO qDay, PLUS
- Prednisone or prednisolone 5 mg PO BID
- Continue until disease progression or unacceptable toxicity
- Refer to prescribing information for abiraterone for dosing information
- Patients receive a GnRH analog concurrently or should have had bilateral orchiectomy
Dosage Modifications
Management of adverse reactions
- Consider dose interruption or dose reduction to manage adverse reactions
-
Tablets
- Recommended dose reduction: 250 mg (one 150-mg tablet and one 100-mg tablet) PO BID
- If a further final dose reduction is required, then reduce to 200 mg (two 100-mg tablets) PO BID
Coadministration with CYP3A inhibitors
- Strong or moderate CYP3A inhibitors: Avoid use, consider alternatives
- If strong CYP3A inhibitors cannot be avoided: Reduce olaparib dose to 100 mg (one 100-mg tablet) PO BID
- If moderate CYP3A inhibitors cannot be avoided: Reduce olaparib dose to 150 mg (one 150-mg tablet) PO BID
Hepatic impairment
- Mild to moderate hepatic impairment (Child-Pugh Class A and B): No dosage adjustment necessary
- Severe hepatic impairment (Child-Pugh Class C): Not studied
Renal impairment
- Mild (CrCl 50-80 mL/min): No dosage adjustment necessary
- Moderate (CrCl 31-50 mL/min): Reduce dose to 200 mg (two 100-mg tablets) BID
- Severe (CrCl <30 mL/min or dialysis): Not evaluated
Dosing Considerations
Withdrawal of capsules
- In 2017, FDA reported olaparib capsules were being phased out of the US market
- Capsules were withdrawn from the market to avoid confusion and potential dosing errors with the tablets, and to reduce the pill burden
Patient selection
- Select for treatment based on presence of deleterious or suspected deleterious HRR gene mutations, including BRCA mutations, or genomic instability based on indication, biomarker, and sample type
- Information on FDA-approved tests is available at http://www.fda.gov/companiondiagnostics
-
Indications supported by diagnostic tests
- Germline or somatic BRCA-mutated advanced ovarian cancer
- HRD-positive advanced ovarian cancer in combination with bevacizumab
- Recurrent ovarian cancer
- Germline BRCA-mutated HER2-negative metastatic breast cancer
- Germline BRCA-mutated metastatic pancreatic adenocarcinoma
- Germline or somatic HRR gene-mutated mCRPC
- BRCA-mutated mCRPC
Safety and efficacy not established
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (0)
Serious - Use Alternative (88)
- amiodarone
amiodarone will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- amobarbital
amobarbital will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- apalutamide
apalutamide will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Coadministration of apalutamide, a strong CYP3A4 inducer, with drugs that are CYP3A4 substrates can result in lower exposure to these medications. Avoid or substitute another drug for these medications when possible. Evaluate for loss of therapeutic effect if medication must be coadministered. Adjust dose according to prescribing information if needed.
- aprepitant
aprepitant will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- atazanavir
atazanavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- bicalutamide
bicalutamide will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- bosentan
bosentan will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inducers cannot be avoided, be aware of a potential for decreased efficacy of olaparib
- carbamazepine
carbamazepine will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- ceritinib
ceritinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- chloramphenicol
chloramphenicol will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- cimetidine
cimetidine will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- ciprofloxacin
ciprofloxacin will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- clarithromycin
clarithromycin will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- cobicistat
cobicistat will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- conivaptan
conivaptan will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- crizotinib
crizotinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- cyclosporine
cyclosporine will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
cyclosporine and olaparib both increase pharmacodynamic synergism. Avoid or Use Alternate Drug. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity. - dabrafenib
dabrafenib will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- danazol
danazol will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- darunavir
darunavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- dexamethasone
dexamethasone will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- diltiazem
diltiazem will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- dronedarone
dronedarone will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- efavirenz
efavirenz will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inducers cannot be avoided, be aware of a potential for decreased efficacy of olaparib
- elvitegravir/cobicistat/emtricitabine/tenofovir DF
elvitegravir/cobicistat/emtricitabine/tenofovir DF will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- enzalutamide
enzalutamide will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- erythromycin base
erythromycin base will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- erythromycin ethylsuccinate
erythromycin ethylsuccinate will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- erythromycin lactobionate
erythromycin lactobionate will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- erythromycin stearate
erythromycin stearate will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- eslicarbazepine acetate
eslicarbazepine acetate will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- etrasimod
etrasimod, olaparib. Either increases effects of the other by immunosuppressive effects; risk of infection. Avoid or Use Alternate Drug. Risk of additive immune system effects with etrasimod has not been studied in combination with antineoplastic, immune-modulating, or noncorticosteroid immunosuppressive therapies. Avoid coadministration during and in the weeks following administration of etrasimod.
- etravirine
etravirine will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inducers cannot be avoided, be aware of a potential for decreased efficacy of olaparib
- fexinidazole
fexinidazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Fexinidazole inhibits CYP3A4. Coadministration may increase risk for adverse effects of CYP3A4 substrates.
- fluconazole
fluconazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- fosamprenavir
fosamprenavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- fosaprepitant
fosaprepitant will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- fosphenytoin
fosphenytoin will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- grapefruit
grapefruit will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- haloperidol
haloperidol will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- idelalisib
idelalisib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- iloperidone
iloperidone will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- imatinib
imatinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- indinavir
indinavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- isoniazid
isoniazid will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- itraconazole
itraconazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- ivosidenib
ivosidenib will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of sensitive CYP3A4 substrates with ivosidenib or replace with alternative therapies. If coadministration is unavoidable, monitor patients for loss of therapeutic effect of these drugs.
- ketoconazole
ketoconazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 100 mg PO BID.
- lapatinib
lapatinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- lenacapavir
lenacapavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of moderate CYP3A4 inhibitors with olaparib (a CYP3A4 substrate). If unavoidable, reduce olaparib dose for tablets to 150 mg BID and reduce olaparib dose for capsules to 200 mg BID. After stopping the inhibitor, wait for 3-5 times the half-life of the inhibitor, and then resume the olaparib dose used before use of inhibitor.
- levoketoconazole
levoketoconazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 100 mg PO BID.
- lidocaine
lidocaine will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- lopinavir
lopinavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- lorlatinib
lorlatinib will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- metronidazole
metronidazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- mifepristone
mifepristone will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If concomitant use necessary, reduce dose of olaparib to 100 mg twice daily; original dose may be resumed 3 to 5 elimination half-lives after mifepristone is discontinued
- mitotane
mitotane will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- nafcillin
nafcillin will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inducers cannot be avoided, be aware of a potential for decreased efficacy of olaparib
- nefazodone
nefazodone will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- nelfinavir
nelfinavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- netupitant/palonosetron
netupitant/palonosetron will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- nevirapine
nevirapine will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- nicardipine
nicardipine will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- oxcarbazepine
oxcarbazepine will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- palifermin
palifermin increases toxicity of olaparib by Other (see comment). Avoid or Use Alternate Drug. Comment: Palifermin should not be administered within 24 hr before, during infusion of, or within 24 hr after administration of antineoplastic agents. Coadministration of palifermin within 24 hr of chemotherapy resulted in increased severity and duration of oral mucositis.
- pentobarbital
pentobarbital will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- phenobarbital
phenobarbital will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- phenytoin
phenytoin will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- posaconazole
posaconazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- primidone
primidone will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- quinidine
quinidine will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- rifabutin
rifabutin will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- rifampin
rifampin will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- rifapentine
rifapentine will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- ritonavir
ritonavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- ropeginterferon alfa 2b
ropeginterferon alfa 2b, olaparib. Either increases toxicity of the other by Other (see comment). Avoid or Use Alternate Drug. Comment: Myelosuppressive agents can produce additive myelosuppression. Avoid use and monitor patients receiving the combination for effects of excessive myelosuppression.
- saquinavir
saquinavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- secobarbital
secobarbital will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug.
- sertraline
sertraline will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- St John's Wort
St John's Wort will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of olaparib with strong CYP3A4 inducers.
- tetracycline
tetracycline will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- ticagrelor
ticagrelor will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- tipranavir
tipranavir will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- tucatinib
tucatinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Avoid concomitant use of tucatinib with CYP3A substrates, where minimal concentration changes may lead to serious or life-threatening toxicities. If unavoidable, reduce CYP3A substrate dose according to product labeling.
- verapamil
verapamil will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
- voriconazole
voriconazole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with strong CYP3A inhibitors cannot be avoided, reduce olaparib dose to 150 mg (capsule) or 100 mg (tablet) PO BID. Do not substitute tablets with capsules.
- voxelotor
voxelotor will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. Voxelotor increases systemic exposure of sensitive CYP3A4 substrates. Avoid coadministration with sensitive CYP3A4 substrates with a narrow therapeutic index. Consider dose reduction of the sensitive CYP3A4 substrate(s) if unable to avoid.
- zileuton
zileuton will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration with moderate CYP3A inhibitors cannot be avoided, reduce olaparib dose to 200 mg (capsule) or 150 mg (tablet) PO BID. Do not substitute tablets with capsules.
Monitor Closely (93)
- abatacept
abatacept and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- adalimumab
adalimumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- alefacept
alefacept and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- alemtuzumab
alemtuzumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- anakinra
anakinra and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- antithymocyte globulin equine
antithymocyte globulin equine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- antithymocyte globulin rabbit
antithymocyte globulin rabbit and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- auranofin
auranofin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- azacitidine
azacitidine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- azathioprine
azathioprine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- basiliximab
basiliximab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- belatacept
belatacept and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- belimumab
belimumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- bleomycin
bleomycin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- busulfan
busulfan and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- C1 inhibitor human
C1 inhibitor human and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- cabazitaxel
cabazitaxel and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- canakinumab
canakinumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- capecitabine
capecitabine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- carboplatin
carboplatin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- carmustine
carmustine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- cenobamate
cenobamate will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Increase dose of CYP3A4 substrate, as needed, when coadministered with cenobamate.
- certolizumab pegol
certolizumab pegol and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- chlorambucil
chlorambucil and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- chloroquine
chloroquine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- cisplatin
cisplatin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- cyclophosphamide
cyclophosphamide and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- cytarabine
cytarabine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- dacarbazine
dacarbazine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- dactinomycin
dactinomycin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- daunorubicin
daunorubicin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- denosumab
denosumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- docetaxel
docetaxel and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- doxorubicin
doxorubicin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- doxorubicin liposomal
doxorubicin liposomal and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- elagolix
elagolix decreases levels of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Elagolix is a weak-to-moderate CYP3A4 inducer. Monitor CYP3A substrates if coadministered. Consider increasing CYP3A substrate dose if needed.
- encorafenib
encorafenib, olaparib. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Encorafenib both inhibits and induces CYP3A4 at clinically relevant plasma concentrations. Coadministration of encorafenib with sensitive CYP3A4 substrates may result in increased toxicity or decreased efficacy of these agents.
- epirubicin
epirubicin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- etanercept
etanercept and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- etoposide
etoposide and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- fedratinib
fedratinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Adjust dose of drugs that are CYP3A4 substrates as necessary.
- fingolimod
fingolimod and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- floxuridine
floxuridine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- fludarabine
fludarabine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- fluorouracil
fluorouracil and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- gemcitabine
gemcitabine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- gemtuzumab
gemtuzumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- gold sodium thiomalate
gold sodium thiomalate and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- golimumab
golimumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- ibritumomab tiuxetan
ibritumomab tiuxetan and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- idarubicin
idarubicin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- ifosfamide
ifosfamide and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- infliximab
infliximab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- irinotecan
irinotecan and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- irinotecan liposomal
irinotecan liposomal and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- istradefylline
istradefylline will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Istradefylline 40 mg/day increased peak levels and AUC of CYP3A4 substrates in clinical trials. This effect was not observed with istradefylline 20 mg/day. Consider dose reduction of sensitive CYP3A4 substrates.
- leflunomide
leflunomide and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- lomustine
lomustine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- mercaptopurine
mercaptopurine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- methotrexate
methotrexate and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- mitoxantrone
mitoxantrone and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- muromonab CD3
muromonab CD3 and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- mycophenolate
mycophenolate and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- natalizumab
natalizumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- nelarabine
nelarabine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- ofatumumab
ofatumumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- ofatumumab SC
ofatumumab SC, olaparib. Either increases effects of the other by immunosuppressive effects; risk of infection. Use Caution/Monitor. Consider the risk of additive immune system effects when coadministering immunosuppressive therapies with coadministration. When switching from therapies with immune effects, take into account the duration and mechanism of action of these therapies when initiating ofatumumab SC.
- oxaliplatin
oxaliplatin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- paclitaxel
paclitaxel and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- paclitaxel protein bound
paclitaxel protein bound and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- pentostatin
pentostatin and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- pralatrexate
pralatrexate and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- ribociclib
ribociclib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely.
- rilonacept
rilonacept and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- rucaparib
rucaparib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Adjust dosage of CYP3A4 substrates, if clinically indicated.
- siponimod
siponimod and olaparib both increase immunosuppressive effects; risk of infection. Use Caution/Monitor. Caution if coadministered because of additive immunosuppressive effects during such therapy and in the weeks following administration. When switching from drugs with prolonged immune effects, consider the half-life and mode of action of these drugs to avoid unintended additive immunosuppressive effects.
- sirolimus
sirolimus and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- stiripentol
stiripentol, olaparib. affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Stiripentol is a CYP3A4 inhibitor and inducer. Monitor CYP3A4 substrates coadministered with stiripentol for increased or decreased effects. CYP3A4 substrates may require dosage adjustment.
- tacrolimus
tacrolimus and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- tazemetostat
tazemetostat will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- tecovirimat
tecovirimat will decrease the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Tecovirimat is a weak CYP3A4 inducer. Monitor sensitive CYP3A4 substrates for effectiveness if coadministered.
- temozolomide
temozolomide and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- temsirolimus
temsirolimus and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- teniposide
teniposide and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- thioguanine
thioguanine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- thiotepa
thiotepa and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- tocilizumab
tocilizumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- topotecan
topotecan and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- ustekinumab
ustekinumab and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- vinblastine
vinblastine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- vincristine
vincristine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- vincristine liposomal
vincristine liposomal and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
- vinorelbine
vinorelbine and olaparib both increase pharmacodynamic synergism. Use Caution/Monitor. Coadministration with other other myelosuppressive anticancer agents, including DNA damaging agents, may potentiate and prolongate the myelosuppressive toxicity.
Minor (5)
- acetazolamide
acetazolamide will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- anastrozole
anastrozole will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- cyclophosphamide
cyclophosphamide will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- drospirenone
drospirenone will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- larotrectinib
larotrectinib will increase the level or effect of olaparib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
Adverse Effects
All grades of severity are listed unless otherwise indicated
>10% (Maintenance Treatment for BRCA-mutated Advanced Ovarian)
Decreased hemoglobin (87%)
Increased mean corpuscular volume (87%)
Nausea (77%)
Decrease leukocytes (70%)
Fatigue (67%)
Decreased lymphocytes (67%)
Decreased ANC (51%)
Abdominal pain (45%)
Vomiting (40%)
Anemia (38%)
Diarrhea (37%)
Decreased platelets (35%)
Increased serum creatinine (34%)
Constipation (28%)
Upper respiratory tract infection (eg, influenza, nasopharyngitis, bronchitis) (28%)
Dysgeusia (26%)
Anemia, Grade 3 or 4 (21%)
Dizziness (20%)
Decreased appetite (20%)
Decreased hemoglobin, Grade 3 or 4 (19%)
Neutropenia (17%)
Dyspepsia (17%)
Dyspnea (15%)
Decreased lymphocytes, Grade 3 or 4 (14%)
Urinary tract infection (13%)
Thrombocytopenia (11%)
Stomatitis (11%)
>10% (Maintenance Treatment for Recurrent Advanced Ovarian)
Increased mean corpuscular volume (89%)
Decreased hemoglobin (83%)
Nausea (76%)
Decreased leukocytes (69%)
Decreased lymphocytes (67%)
Fatigue (66%)
Decreased ANC (51%)
Anemia (44%)
Increased serum creatinine (44%)
Decreased platelets (42%)
Vomiting (37%)
Upper respiratory tract infection (36%)
Diarrhea (33%)
Arthralgia/myalgia (30%)
Dysgeusia (27%)
Headache (26%)
Decreased appetite (22%)
Stomatitis (20%)
Neutropenia (19%)
Cough (18%)
Leukopenia (16%)
Hypomagnesemia (14%)
Thrombocytopenia (14%)
Dizziness (13%)
Dyspepsia (11%)
Increased creatinine (11%)
1-10% (BRCA-mutated Advanced Ovarian)
Maintenance treatment
- Neutropenia, Grade 3 or 4 (6%)
- Fatigue, Grade 3 or 4 (4%)
- Leukopenia, Grade 3 or 4 (3%)
- Diarrhea, Grade 3 or 4 (3%)
- Abdominal pain, Grade 3 or 4 (2%)
- Thrombocytopenia, Grade 3 or 4 (1%)
- Nausea, Grade 3 or 4 (1%)
1-10% (Maintenance Treatment for Recurrent Advanced Ovarian)
Edema (8%)
Rash (6%)
Fatigue, Grade 3 or 4 (4%)
Nausea, Grade 3 or 4 (3%)
Vomiting, Grade 3 or 4 (3%)
Diarrhea, Grade 3 or 4 (2%)
Lymphopenia (1%)
Headache, Grade 3 or 4 (1%)
Stomatitis, Grade 3 or 4 (1%)
Postmarketing Reports
Hypersensitivity (rash, dermatitis, angioedema)
Cough
Thrombocytopenia
Dysgeusia
Lymphopenia
Dizziness
Stomatitis
Upper abdominal pain
Erythema nodosum, rash, dermatitis
Venous thromboembolic events
Warnings
Contraindications
None
Cautions
Pneumonitis, including fatal cases, occurred in <1%; interrupt treatment if pneumonitis is suspected; discontinue if pneumonitis is confirmed; if patients present with new or worsening respiratory symptoms such as dyspnea, cough and fever, or a radiological abnormality occurs, interrupt treatment and promptly assess source of symptoms; if pneumonitis confirmed, discontinue treatment and treat patient appropriately
Can cause fetal harm when administered to a pregnant woman based on its mechanism of action and findings in animals; (see Pregnancy)
Venous thromboembolic events, including severe or fatal pulmonary embolism, occurred in mCRPC patients who were treated with olaparib and androgen deprivation therapy; monitor for signs and symptoms of venous thrombosis and pulmonary embolism and treat as medically appropriate, which may include long-term anticoagulation as clinically indicated
Myelodysplastic syndrome/ acute myeloid leukemia
- Myelodysplastic syndrome/acute myeloid leukemia (MDS/AML) occurred in clinical trials
- Advise patients to contact their healthcare provider if they experience weakness, feeling tired, fever, weight loss, frequent infections, bruising, bleeding easily, breathlessness, blood in urine or stool, and/or laboratory findings of low blood cell counts, or a need for blood transfusions
- Monitor complete blood cell count for cytopenia at baseline and monthly thereafter for clinically significant changes during treatment
- Do not initiate treatment until hematological toxicity caused by previous chemotherapy (Grade ≤1) resolves
- For prolonged hematological toxicities, interrupt treatment and promptly assess source of symptoms; monitor blood counts weekly until recovery
- If levels have not recovered to Grade ≤1 after 4 weeks, refer to a hematologist for further investigations, including bone marrow analysis and blood sample for cytogenetics
- All patients with myelodysplastic syndrome reported to have received previous chemotherapy with platinum agents and/or other DNA damaging agents including radiotherapy; some of these patients also had a history of more than one primary malignancy or of bone marrow dysplasia
- If MDS/AML is confirmed, discontinue olaparib
Drug interactions overview
- Clinical studies of olaparib in combination with other myelosuppressive anticancer agents (eg, DNA damaging agents) indicate a potentiation and prolongation of myelosuppressive toxicity
-
CYP3A4 inhibitors
- Olaparib is a CYP3A4 substrate; coadministration of strong or moderate CYP3A4 inhibitors may increase olaparib plasma concentrations
- Avoid concomitant use of strong or moderate CYP3A inhibitors (see Dosage Modifications)
- If strong or moderate CYP3A inhibitors must be coadministered, reduce dose of olaparib (see Dosage Modifications)
- Avoid grapefruit, grapefruit juice, Seville oranges and Seville orange juice during olarparib treatment since they are CYP3A inhibitors
-
CYP3A4 inducers
- Coadministration of strong or moderate CYP3A4 inducers may decrease olaparib plasma concentrations
- Avoid concomitant use of strong or moderate CYP3A inducers
- If a strong or moderate CYP3A inducer cannot be avoided, be aware of a potential for decreased efficacy of olaparib (see Dosage Modifications)
Pregnancy & Lactation
Pregnancy
Based on findings in animals and mechanism of action, fetal harm may occur when administered to a pregnant woman; there are no available data on use in pregnant women to inform of drug associated risk
Olaparib was teratogenic and caused embryo-fetal toxicity in rats at exposures below those in patients receiving the recommended human dose of 400 mg BID
Contraception
- In women of childbearing potential, avoid pregnancy by using effective contraception during treatment and for at least 6 month after receiving the last dose; pregnancy testing is recommended for females of reproductive potential prior to initiating treatment
- Based on findings in genetic toxicity and animal reproduction studies, advise male patients with female partners of reproductive potential or who are pregnant to use effective contraception during treatment and for 3 months following the last dose of olaparib
- Advise male patients not to donate sperm during therapy and for 3 months following the last dose of olaparib
Lactation
No data are available regarding presence of olaparib in human milk, or on effects on breastfed infant or on milk production; because of potential for serious adverse reactions in breastfed infants from therapy, advise lactating women not to breastfeed during treatment and for 1 month after receiving last dose
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of Action
Inhibitor of poly (ADP-ribose) polymerase (PARP) enzymes, including PARP1, PARP2, and PARP3
PARP enzymes are involved in normal cellular homeostasis, such as DNA transcription, cell cycle regulation, and DNA repair
Absorption
Bioavailability of tablet formulation is higher than the capsule formulation (AUC at steady-state 77% higher with tablet)
Peak plasma time: 1.5 hr (tablet); 1-3 hr (capsule)
Peak plasma concentration: 7.7 mcg/mL (tablet at steady-state)
AUC: 49 mcg·hr/mL (tablet at steady-state)
Steady-state achieved: 3-4 days
Coadministration with a high-fat meal slowed the rate (Peak plasma time delayed by 2.5 hr [tablet] or 2 hr [capsule]) of absorption, but did not significantly alter the extent of absorption (mean AUC increased by ~8% [tablet] or ~20% [capsule])
Distribution
Protein bound: 82%
Vd: 158 L (tablet); 167 L (capsule)
Metabolism
Metabolized primarily by CYP3A4/5
Elimination
Half-life: 14.9 hr (tablet); 11.9 hr (capsule)
Plasma clearance: 7.4 L/hr (tablet); 8.6 L/hr (capsule)
Excretion: 44% urine; 42% feces
Excreted mostly as metabolites
Pharmacogenomics
Indicated as monotherapy in patients with deleterious or suspected deleterious germline BRCA-mutated (as detected by an FDA-approved test) advanced ovarian cancer or breast cancer
Information on FDA-approved test for the detection of BRCA mutations is available at http://www.fda.gov/companiondiagnostics
Administration
Oral Administration
To avoid substitution errors and overdose, do not substitute olaparib tablets with olaparib capsules on a mg-to-mg basis due to differences in the dosing and bioavailability of each formulation
May take with or without food
Swallow tablets whole; do not chew, crush, dissolve or divide
Missed dose: Instruct patient to take their next dose at its scheduled time
Storage
Tablets: Store at 20-25ºC (68-77°F), excursions permitted to 15-30ºC (59-86°F)
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| Lynparza oral - | 100 mg tablet |  | |
| Lynparza oral - | 150 mg tablet | 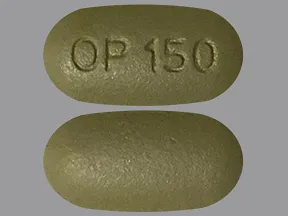 |
Copyright © 2010 First DataBank, Inc.
Patient Handout
olaparib oral
OLAPARIB CAPSULE - ORAL
(oh-LAP-a-rib)
COMMON BRAND NAME(S): Lynparza
USES: This medication is used to treat ovarian cancer. It works by slowing the growth of cancer cells.
HOW TO USE: Read the Medication Guide provided by your pharmacist before you start taking olaparib and each time you get a refill. If you have any questions, ask your doctor or pharmacist.This medication also comes in a tablet form. Do not take the tablet form in place of the capsules unless your doctor tells you to do so. They do not work the same way. Ask your doctor for details.Take this medication by mouth with or without food as directed by your doctor, usually twice daily. Swallow the capsules whole. Do not chew, dissolve, or open the capsules. Do not take capsules that look damaged or look like they have leaked.Avoid eating grapefruit or drinking grapefruit juice while using this medication unless your doctor or pharmacist says you may do so safely. Also avoid eating Seville oranges (often found in marmalade). Grapefruit and Seville oranges can increase the chance of side effects with this medicine. Ask your doctor or pharmacist for more details.The dosage is based on your medical condition and response to treatment.Do not increase your dose or use this drug more often or for longer than prescribed. Your condition will not improve any faster, and your risk of serious side effects will increase.Since this drug can be absorbed through the skin and lungs and may harm an unborn baby, women who are pregnant or who may become pregnant should not handle this medication or breathe the dust from the capsules.
SIDE EFFECTS: Nausea, vomiting, loss of appetite, diarrhea, constipation, bad taste in your mouth, dizziness, or joint/back/muscle pain may occur. Rarely, nausea and vomiting can be severe. In some cases, your doctor may prescribe medication to prevent or relieve nausea and vomiting. Eating several small meals or limiting activity may help lessen nausea and vomiting. If any of these effects last or get worse, tell your doctor or pharmacist promptly.Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Tell your doctor right away if you have any serious side effects, including: signs of kidney problems (such as change in the amount of urine), swelling hands/ankles/feet.This medication decreases bone marrow function, an effect that may lead to a low number of blood cells such as red cells, white cells, and platelets. This effect can cause anemia, decrease your body's ability to fight an infection, or cause easy bruising/bleeding. Rarely, these problems can also be symptoms of very serious (possibly fatal) cancer of the bone marrow or blood cells, especially if you have received past radiation or chemotherapy treatment for ovarian cancer. Your doctor will monitor your blood cell counts. Tell your doctor right away if you develop any of the following symptoms: signs of anemia (such as unusual tiredness, pale skin, rapid breathing, fast heartbeat), signs of infection (such as sore throat that doesn't go away, fever, chills), easy bruising/bleeding (such as pink/bloody urine, black/bloody stools), weakness, weight loss.Get medical help right away if you have any very serious side effects, including: new/worsening shortness of breath, cough, wheezing.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US -Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before taking olaparib, tell your doctor or pharmacist if you are allergic to it; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.Before using this medication, tell your doctor or pharmacist your medical history, especially of: kidney disease.Olaparib can make you more likely to get infections or may make current infections worse. Stay away from anyone who has an infection that may easily spread (such as chickenpox, COVID-19, measles, flu). Talk to your doctor if you have been exposed to an infection or for more details.Tell your health care professional that you are using olaparib before having any immunizations/vaccinations. Avoid contact with people who have recently received live vaccines (such as flu vaccine inhaled through the nose).To lower the chance of getting cut, bruised, or injured, use caution with sharp objects like razors and nail cutters, and avoid activities such as contact sports.This drug may make you dizzy. Alcohol or marijuana (cannabis) can make you more dizzy. Do not drive, use machinery, or do anything that needs alertness until you can do it safely. Limit alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).Men should not donate sperm while using olaparib and for 3 months after stopping treatment.Tell your doctor if you are pregnant or plan to become pregnant. You should not become pregnant while using olaparib. Olaparib may harm an unborn baby. Your doctor should order a pregnancy test before you start this medication. Women using this medication should ask about reliable forms of birth control during treatment and for at least 6 months after the last dose. Men using this medication should ask about reliable forms of birth control during treatment and for at least 3 months after the last dose. If you become pregnant, talk to your doctor right away about the risks and benefits of this medication.Since this drug can be absorbed through the skin and lungs and may harm an unborn baby, women who are pregnant or who may become pregnant should not handle this medication or breathe the dust from the capsules.It is unknown if this drug passes into breast milk. Because of the possible risk to the infant, breastfeeding is not recommended while using this drug and for at least one month after the last dose. Consult your doctor before breastfeeding.
DRUG INTERACTIONS: See also How to Use section.Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.Other medications can affect the removal of olaparib from your body, which may affect how olaparib works. Examples include carbamazepine, phenytoin, rifamycins (such as rifampin), St. John's wort, among others.
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call 1-800-222-1222. Canada residents can call 1-844-764-7669.
NOTES: Do not share this medication with others.Lab and/or medical tests (such as complete blood counts) should be done while you are taking this medication. Keep all medical and lab appointments. Consult your doctor for more details.
MISSED DOSE: If you miss a dose, take it as soon as you remember. If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
STORAGE: Store in the refrigerator. Do not freeze. If needed, this medication may be stored at room temperature away from light and moisture for up to 3 months. Do not store in the bathroom. Do not use this medication if it has been exposed to temperatures above 104 degrees F (40 degrees C) or if it has been frozen. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
MEDICAL ALERT: Your condition can cause complications in a medical emergency. For information about enrolling in MedicAlert, call 1-888-633-4298 (US) or 1-800-668-1507 (Canada).
Information last revised May 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.


