To determine whether breaking up prolonged sitting with short bouts of standing or walking improves postprandial markers of cardiometabolic health in women at high risk of type 2 diabetes.
Twenty-two overweight/obese, dysglycemic, postmenopausal women (mean ± SD age 66.6 ± 4.7 years) each participated in two of the following treatments: prolonged, unbroken sitting (7.5 h) or prolonged sitting broken up with either standing or walking at a self-perceived light intensity (for 5 min every 30 min). Both allocation and treatment order were randomized. The incremental area under the curves (iAUCs) for glucose, insulin, nonesterified fatty acids (NEFA), and triglycerides were calculated for each treatment condition (mean ± SEM). The following day, all participants underwent the 7.5-h sitting protocol.
Compared with a prolonged bout of sitting (iAUC 5.3 ± 0.8 mmol/L ⋅ h), both standing (3.5 ± 0.8 mmol/L ⋅ h) and walking (3.8 ± 0.7 mmol/L ⋅ h) significantly reduced the glucose iAUC (both P < 0.05). When compared with prolonged sitting (548.2 ± 71.8 mU/L ⋅ h), insulin was also reduced for both activity conditions (standing, 437.2 ± 73.5 mU/L ⋅ h; walking, 347.9 ± 78.7 mU/L ⋅ h; both P < 0.05). Both standing (−1.0 ± 0.2 mmol/L ⋅ h) and walking (−0.8 ± 0.2 mmol/L ⋅ h) attenuated the suppression of NEFA compared with prolonged sitting (−1.5 ± 0.2 mmol/L ⋅ h) (both P < 0.05). There was no significant effect on triglyceride iAUC. The effects on glucose (standing and walking) and insulin (walking only) persisted into the following day.
Breaking up prolonged sitting with 5-min bouts of standing or walking at a self-perceived light intensity reduced postprandial glucose, insulin, and NEFA responses in women at high risk of type 2 diabetes. This simple, behavioral approach could inform future public health interventions aimed at improving the metabolic profile of postmenopausal, dysglycemic women.
Introduction
Sedentary behavior, now commonly conceptualized as sitting during waking hours with low energy expenditure (1), has recently emerged as an independent determinant of morbidity (particularly type 2 diabetes) and mortality (2–4). Multiple observational studies have also demonstrated a positive association between objectively measured sedentary time and markers of diabetes risk, independent of the amount of moderate-to-vigorous physical activity (MVPA) undertaken (5–7). This suggests that sedentary behavior is likely to be a distinct risk factor for type 2 diabetes and a potential target for lifestyle intervention. This is important, as individuals at high risk of type 2 diabetes spend ∼70% of their waking time sedentary, with 25% in light activity and <5% engaged in MVPA (6). Moreover, the inverse correlation between sedentary behavior and MVPA is weak (7), further suggesting these are independent behaviors. However, experimental data are needed to determine whether a causal relationship exists between modifications to sedentary time and metabolic health.
Recently, experimental studies that have broken up prolonged sitting with short periods of light- or moderate-intensity activity have shown a reduction in postprandial glucose and insulin concentrations in both healthy and overweight adults (8–11). These studies suggest that important health-related metabolic processes occur when individuals transition from sitting to movement (light and moderate intensity). However, it is unclear whether moving from sitting to standing provides a sufficient stimulus to elicit metabolic benefits. While there is emerging evidence that sustained bouts of standing may improve glucose regulation (12,13), it is not clear whether breaking up prolonged sitting with intermittent short bouts of standing improves the metabolic health of individuals at high risk of chronic disease.
Therefore, the aim of this study was to establish whether breaking up prolonged sitting through frequent short bouts of standing or walking activity modulates postprandial metabolic responses in individuals at high risk of type 2 diabetes.
Research Design and Methods
Study Design
A balanced incomplete block design was used for this study (14). Such designs have been used in pharmaceutical trials and reduce participant burden while minimizing the intrasubject effect, thus increasing the sensitivity of the outcome (15,16). With this design, participants were randomized to two of the three following treatment conditions: 1) prolonged, unbroken sitting (7.5 h); 2) prolonged sitting broken up with standing for 5 min every 30 min; or 3) prolonged sitting broken up with walking for 5 min every 30 min (Supplementary Table 1). Regardless of the treatment condition carried out on day 1, all participants underwent the prolonged sitting protocol on day 2; thus, each treatment condition was carried out over 2 consecutive days. As an acute bout of physical activity may enhance insulin sensitivity for up to 48 h (17), we used a minimum washout period of 7 days between each condition (the maximum washout was 22 days).
Participants attended five separate visits to the Leicester Diabetes Centre, Leicester, U.K. Supplementary Fig. 1 describes the study design. One to two weeks after an initial familiarization visit, participants were randomized by an independent third party to one of six sequences, prepared by the study statistician prior to recruitment of the first participant (Supplementary Table 1).
Informed consent was obtained from all eligible participants, and ethics approval was obtained from the Northampton Research Ethics Committee.
Participants
A total of 34 participants were recruited between January 2014 and October 2014. Postmenopausal women at high risk of developing type 2 diabetes were identified from studies previously conducted within the Leicester Diabetes Centre (18,19). This cohort was included in order to negate the impact of hormone variations and because associations between sedentary behavior and markers of cardiometabolic health have previously been shown to be stronger in women (20).
Eligibility criteria included the following: overweight or obese (BMI ≥27.5 kg/m2 or ≥25 kg/m2 if South Asian), postmenopausal women (12 consecutive months without menstruation [21]), age 50–75 years with screen-detected impaired glucose regulation identified within the 12 months prior to the invitation letter being sent. Impaired glucose regulation was defined as 2-h postchallenge glucose ≥7.8 mmol/L to <11.1 mmol/L after a standard oral glucose tolerance test (22) or HbA1c between 5.7 and 6.4% (39–46 mmol/mol) inclusive (23). Exclusion criteria were regular purposeful exercise (≥150 min of objectively measured MVPA over a typical week), inability to communicate in spoken English, steroid use, known type 2 diabetes, or current use of hormone replacement medication.
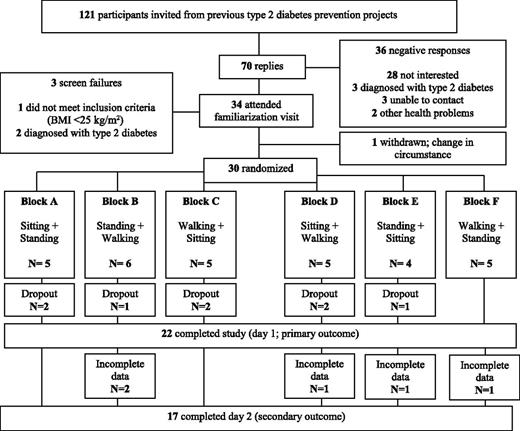
In total, 30 participants were randomized (Fig. 1). Causes of dropout between familiarization and randomization are detailed in Fig. 1. A further eight individuals were excluded after randomization, due to cessation of the venous cannula line, which resulted in <50% of data collection (n = 5), illness (n = 2), or a change in personal circumstance (n = 1). This left 22 participants who were included in the analysis. There were no significant differences in BMI, age, or HbA1c between those who dropped out or were excluded and those who were included in the study.
Familiarization Visit
Before participating in the experimental protocol, all participants visited the Leicester Diabetes Centre for a familiarization visit where they provided informed consent. This allowed participants to become accustomed to the walking speed and also familiarize themselves with the Borg rating of perceived exertion (RPE) scale (24). A venous blood sample was also taken for HbA1c, lipid profile, and nonesterified fatty acid (NEFA) analysis.
Body mass (Tanita TBE 611; Tanita, West Drayton, U.K.), waist circumference (midpoint between the lower costal margin and iliac crest), and height were measured to the nearest 0.1 kg, 0.5 cm, and 0.5 cm, respectively.
Participants also wore an accelerometer (placed on the right anterior axillary line) for 7 days after familiarization (GT3X+; ActiGraph, Pensacola, FL) to measure time spent engaged in sedentary, light physical activity, or MVPA under free-living conditions.
Experimental Regimen Overview
Participants were asked to record all food and drink consumed the day before the first experimental condition. They were then asked to replicate this diet before subsequent treatments. Participants were also requested to avoid alcohol, caffeine, and any MVPA for 2 days prior to each experimental condition.
Participants arrived at the laboratory by car (0800 h) after a 10-h fast and had a cannula fitted into an accessible vein. A fasting blood sample (9 mL) was then taken (time point −1 h) for the quantification of glucose, insulin, NEFA, and triglycerides. Participants were asked to sit quietly for 60 min, and a further 9-mL blood sample was taken. A standardized mixed-meal breakfast (croissant, butter, cheese, double cream, skimmed milk, and a meal-replacement drink [Complan; Nutricia Limited, Wiltshire, U.K.]) was consumed (0900 h; 0 h) providing 0.66 g fat, 0.66 g carbohydrate, and 0.4 g protein/kg body mass (58% fat, 26% carbohydrate, and 16% protein). The time taken to consume the meal (≤15 min) was recorded and replicated in subsequent conditions. Blood was sampled again at 30, 60, 120, and 180 min postprandially. Lunch, with a nutrient composition identical to that of breakfast, was consumed at 1200 h, with blood samples at 30, 60, 120, 180, and 210 min postprandially. The research staff supervised participants throughout each study cycle to ensure full compliance with the trial protocols. Participants consumed water ad libitum during the first of the experimental conditions and were then asked to replicate the volume ingested in subsequent conditions.
Experimental Regimens: Day 1
Experimental Condition: Prolonged Sitting (7.5 h)
During the prolonged sitting condition, walking and standing were restricted (lavatory visits were conducted via a wheelchair). Participants sat in a designated room equipped with a chair and desk and access to books, magazines, and Internet services.
Experimental Condition: Sitting (Total 6.5 h) Plus Standing (Total 60 min)
This followed the same procedure as the sitting condition except that participants were instructed to break their sitting time by standing close to their chair for 5 min every 30 min. Individuals were asked to stand in the same, fixed position. In total, individuals accumulated 12 bouts (60 min) of standing.
Experimental Condition: Sitting (Total 6.5 h) Plus Walking (Total 60 min)
This was similar to the standing condition, but sitting time was punctuated with 5-min bouts of walking at a self-perceived light intensity on a treadmill (Spazio Forma Folding Treadmill; TechnoGym U.K. Ltd., Bracknell, U.K.). During the first bout of walking, participants were gradually taken up to a speed that registered between 10 and 12 on the Borg RPE scale (24), up to a maximum of 4.0 km/h. This speed was fixed and replicated for all other intervals. In total, individuals accumulated 12 bouts (60 min) of walking.
The average treadmill speed during the walking condition was 3.0 km/h (range 1.5–4.0), with an average RPE score of 10 (range 8–12).
Experimental Regimens: Day 2 (Prolonged Sitting: 7.5 h)
For determination of whether any acute effects of standing and walking persisted into the next day, participants returned to the laboratory (0800 h) after another 10-h fast to undergo the prolonged sitting protocol (including the same standardized meals and timings). They were asked to consume exactly the same meal as the previous evening, while again avoiding alcohol, caffeine, and MVPA.
Sedentary Behavior, Physical Activity, and Posture Data
Participants were asked to wear an accelerometer (GT3X+) and an activPAL3 professional physical activity monitor (PAL Technologies, Glasgow, Scotland) during experimental conditions and an accelerometer for 7 days before each experimental condition (Supplementary Fig. 1).
ActivPAL proprietary software (activPAL Professional V5.9.1.1) was used to create processed csv files.
For accelerometer data collected over each 7-day period, nonwear time was defined as a minimum of 60 min of continuous zero counts, and days with at least 10 h of wear time were considered valid (5,6). In order to be classed as valid, at least 3 days were required (25). Freedson cut points were used to categorize activity intensity (26). Accelerometer data were analyzed using a bespoke tool (KineSoft, version 3.3.76; KineSoft, New Brunswick, Canada [www.kinesoft.org]).
Biochemical Analysis
Plasma glucose and serum triglyceride concentrations were determined using standard enzymatic techniques with commercially available kits (Beckman, High Wycombe, U.K.). The measurement of plasma NEFA involved a three-stage colorimetric assay using a commercially available kit (RX monza; Randox Laboratories, County Antrim, U.K.). Glucose, triglycerides, and NEFA were analyzed on the day of collection.
Insulin samples underwent centrifugation to separate plasma within 15 min of collection. Plasma was stored at −80°C and analyzed at the end of data collection using an enzyme immunoassay (Mercodia, Uppsala, Sweden). All measurements and analysis were undertaken by individuals blinded to experimental condition and independent of the scientific advisory team.
Sample Size
The primary outcome was incremental postprandial area under the glucose curve (iAUC) on day 1. Allowing for an intervention effect of a 20% change in glucose iAUC, a standardized difference of 1 (where the SD is equivalent to the anticipated intervention effect), a within-person correlation of 0.3, 90% power, and an α of 0.025 (allowing for two primary comparisons against control conditions), we estimated that we would require 12 participants for a complete three-treatment, three-period crossover design. Twice as many participants were required for the three-treatment, two-period balanced incomplete block design (27), and a 20% dropout rate was allowed for; therefore, we aimed to recruit 30 participants with 24 needed to complete the trial. Estimates were based on previous experimental research (8) and with consideration given to the high-risk nature of our cohort where a greater effect was anticipated.
Statistical Analyses
In line with best practice for acute studies where fasting physiology does not change, outcomes were calculated as iAUC rather than total AUC (28). Values were determined using the trapezium rule and by subtracting fasting levels from the overall postprandial response.
Participants were excluded if they had >50% of blood samples missing across any treatment condition (n = 5). Missing outcome data for remaining participants were imputed using a regression model with key predictor variables (BMI, age, fasting values, ethnicity, and treatment) for each time point and outcome. Imputation was used to correct for verification bias (29). Across all experimental conditions, 11% of data values (378 of 3,472) were missing and imputed (Supplementary Table 2). On average, participants were missing a median of 2 (interquartile range 1–4) values across all experimental days and biochemical variables.
Multilevel mixed-effects linear regression was used to look at the difference between groups in the continuous outcome measures (glucose, insulin, NEFA, triglycerides) allowing for repeated measurements from the same individuals. In these models, treatment was modeled as a fixed factor and participant as a random factor. The primary analysis involved comparing standing and walking against the control (prolonged sitting) condition. Tests between treatment conditions (standing vs. walking) were conducted for exploratory purposes and form a secondary outcome for the study.
All data were analyzed using STATA (version 13.0; StataCorp, College Station, TX). A P value of <0.05 was considered statistically significant. Descriptive data are reported as mean ± SD unless otherwise stated and as mean ± SEM in Figs. 2 and 3 and Supplementary Tables 3–6.
The effect of sitting, standing, and walking on glucose (A), insulin (B), NEFA (C), and triglyceride (D) levels on day 1 (n = 22).
The effect of sitting, standing, and walking on glucose (A), insulin (B), NEFA (C), and triglyceride (D) levels on day 1 (n = 22).
The effect of sitting, standing, and walking on glucose (A), insulin (B), NEFA (C), and triglyceride (D) levels on day 2 (n = 17). Mean ± SEM glucose, insulin, NEFA, and triglycerides on day 1 (Fig. 2A–D) and day 2 (A–D) measured over a 6.5-h period during the prolonged sitting, sitting and standing, and sitting and walking conditions. Standardized meals provided at 0 h and 3 h.
The effect of sitting, standing, and walking on glucose (A), insulin (B), NEFA (C), and triglyceride (D) levels on day 2 (n = 17). Mean ± SEM glucose, insulin, NEFA, and triglycerides on day 1 (Fig. 2A–D) and day 2 (A–D) measured over a 6.5-h period during the prolonged sitting, sitting and standing, and sitting and walking conditions. Standardized meals provided at 0 h and 3 h.
In order to aid interpretation of the results, a sensitivity analysis was conducted to investigate whether results were affected by analyzing the total AUC (including fasting values). Furthermore, we also investigated whether fasting values differed between day 1 and day 2 (Supplementary Table 7).
Results
Anthropometric, biochemical, and demographic information of the included participants is displayed in Table 1.
Metabolic, demographic, and anthropometric characteristics at baseline and dietary and physical activity variables during the study (n = 22)
| Baseline characteristics | |
| Age (years) | 66.6 ± 4.7 |
| Current smoker | 1 (4.5) |
| BMI (kg/m2) | 32.9 ± 4.7 |
| Waist circumference (cm) | 102 ± 9.0 |
| Body mass (kg) | 83.6 ± 11.7 |
| Total cholesterol (mmol/L) | 5.60 ± 0.87 |
| Triglycerides (mmol/L) | 2.17 ± 0.86 |
| NEFA (mmol/L) | 0.44 ± 0.24 |
| HbA1c (%) | 5.8 ± 0.2 |
| HbA1c (mmol/mol) | 40 ± 2.3 |
| Fasting plasma glucose (mmol/L) | 5.4 ± 0.4 |
| Lipid-lowering medication | 5 (22.7) |
| β-Blockers | 5 (22.7) |
| ACE inhibitors | 3 (13.6) |
| Ethnicity | |
| White European | 20 (90.9) |
| Black and minority ethnic | 2 (9.1) |
| In-study characteristics | |
| Diet | |
| Total energy intake (kcal/day) | 1,717 ± 234 |
| Total fat (energy %) | 58 ± 0.2 |
| Total carbohydrate (energy %) | 26 ± 0.1 |
| Total protein (energy %) | 16 ± 0.2 |
| Walking speed (km/h) | 3.0 (1.5–4.0) |
| Borg RPE score | 10 (8–12) |
| Baseline characteristics | |
| Age (years) | 66.6 ± 4.7 |
| Current smoker | 1 (4.5) |
| BMI (kg/m2) | 32.9 ± 4.7 |
| Waist circumference (cm) | 102 ± 9.0 |
| Body mass (kg) | 83.6 ± 11.7 |
| Total cholesterol (mmol/L) | 5.60 ± 0.87 |
| Triglycerides (mmol/L) | 2.17 ± 0.86 |
| NEFA (mmol/L) | 0.44 ± 0.24 |
| HbA1c (%) | 5.8 ± 0.2 |
| HbA1c (mmol/mol) | 40 ± 2.3 |
| Fasting plasma glucose (mmol/L) | 5.4 ± 0.4 |
| Lipid-lowering medication | 5 (22.7) |
| β-Blockers | 5 (22.7) |
| ACE inhibitors | 3 (13.6) |
| Ethnicity | |
| White European | 20 (90.9) |
| Black and minority ethnic | 2 (9.1) |
| In-study characteristics | |
| Diet | |
| Total energy intake (kcal/day) | 1,717 ± 234 |
| Total fat (energy %) | 58 ± 0.2 |
| Total carbohydrate (energy %) | 26 ± 0.1 |
| Total protein (energy %) | 16 ± 0.2 |
| Walking speed (km/h) | 3.0 (1.5–4.0) |
| Borg RPE score | 10 (8–12) |
Data are mean ± SD, n (%), or mean (range).
Experimental Regimens: Day 1
Biochemical results collected on day 1 (for each experimental condition) are presented in Fig. 2, with the corresponding numerical values displayed in Supplementary Table 3.
The mean glucose iAUC response was 5.3 ± 0.8 mmol/L ⋅ h in the prolonged sitting condition. Breaking sitting time with 5 min of standing, every 30 min, reduced the glucose iAUC by 34% (3.5 ± 0.8 mmol/L ⋅ h, P = 0.022) compared with prolonged sitting. Similarly, walking reduced the glucose iAUC by 28% (3.8 ± 0.7 mmol/L ⋅ h, P = 0.009) compared with prolonged sitting.
A similar pattern of results was observed for insulin and NEFA on day 1. The insulin iAUC was reduced by 20% (437.2 ± 73.5 mU/L ⋅ h, P = 0.045) when sitting time was broken with standing and by 37% (347.9 ± 78.7 mU/L ⋅ h, P = 0.008) when it was broken with walking compared with prolonged sitting (548.2 ± 71.8 mU/L ⋅ h). Breaking sitting time with standing attenuated the suppression of the NEFA iAUC by 33% (−1.0 ± 0.2 mmol/L ⋅ h, P = 0.024) and with walking by 47% (−0.8 ± 0.2 mmol/L ⋅ h, P = 0.003) compared with prolonged sitting (−1.5 ± 0.2 mmol/L ⋅ h).
There were no significant differences between the standing and walking conditions for any of these outcomes (glucose P = 0.717, insulin P = 0.376, NEFA P = 0.398).
Conversely, neither standing (6.2 ± 0.8 mmol/L ⋅ h) nor walking (6.1 ± 0.8 mmol/L ⋅ h) significantly reduced the triglyceride iAUC compared with the sitting condition (5.6 ± 0.7 mmol/L ⋅ h) on day 1.
Experimental Regimens: Day 2 (Prolonged Sitting: 7.5 h)
Seventeen participants completed the second day owing to problems with intravenous cannulation. Biochemical results for day 2 are presented in Fig. 3, with the corresponding numerical values displayed in Supplementary Table 4.
Day 2 yielded a mean net glucose response of 4.8 ± 0.6 mmol/L ⋅ h if participants had undertaken the sitting condition on day 1. Breaking sitting time with standing on day 1 elicited a response of 3.9 ± 0.8 mmol/L ⋅ h on day 2 (19% reduction in iAUC compared with sitting, P = 0.039). Similarly, walking carried out on day 1 reduced the glucose iAUC by 17% on day 2 (4.0 ± 0.7 mmol/L ⋅ h, P = 0.027). There was no significant difference between the standing and walking conditions (P = 0.877).
The mean net insulin response was 464.6 ± 70.2 mU/L ⋅ h if participants had undertaken the sitting condition on day 1. The significant results for standing on day 1 did not persist into the second day (363.5 ± 57.5 mU/L ⋅ h, P = 0.325). In contrast, results for walking persisted into day 2 (354.3 ± 57.3 mU/L ⋅ h, P = 0.038). There was no significant difference between the standing and walking conditions (P = 0.529).
There was no difference in triglyceride response between the prolonged sitting (7.2 ± 0.5 mmol/L ⋅ h) and standing (7.2 ± 0.8 mmol/L ⋅ h, P = 0.603) conditions on day 2. Results for the walking condition (6.0 ± 0.7 mmol/L ⋅ h, P = 0.077) neared significance compared with prolonged sitting.
The effects of standing and walking on NEFA were no longer significant on day 2 (standing, −1.0 ± 0.3 mmol/L ⋅ h, P = 0.161; walking, −1.0 ± 0.3 mmol/L ⋅ h, P = 0.144) compared with prolonged sitting (−1.5 ± 0.2 mmol/L ⋅ h).
Sensitivity Analysis
The pattern of results and significance levels were largely unaffected if the data were analyzed using total AUC on day 1 (Supplementary Table 5). However, total AUC on day 2 failed to reach significance for both glucose (standing and walking condition) and insulin (standing only) (Supplementary Table 6). Conversely, results for NEFA became significant for both standing and walking. There were no significant differences between any fasting values on day 1 or day 2 (Supplementary Table 7).
Sedentary and Physical Activity Data
Free-living accelerometer data collected after the familiarization visit (n = 22) (Supplementary Table 8) showed that participants spent 594 ± 80 min/day sedentary (71.5% of total wear time) and only engaged in modest amounts of MVPA (19 ± 10 min/day; 2% of total wear time); there was no difference in these behaviors for the 7 days prior to each experimental conditions (P > 0.05).
The ActiGraph and activPAL monitor data recorded during the experimental conditions confirmed that compliance with the protocol was high (Supplementary Tables 8 and 9). Participants took an average 6 ± 2 steps and 252 ± 18 steps during each 5-min standing and walking bout, respectively.
Conclusions
In overweight, postmenopausal women with dysglycemia, we observed that interrupting periods of prolonged sitting with 5 min of standing every 30 min elicits changes to postprandial glucose metabolism similar to those associated with breaking up sitting with identical periods of self-perceived light-intensity walking. Compared with uninterrupted sitting, standing reduced the postprandial rise in glucose by 34% (compared with a 28% reduction for walking) and the postprandial rise in insulin concentrations by 20% (37% for walking) on the day of the intervention. Moreover, the observations for glucose (standing and walking) and insulin (walking only) persisted into the next day.
These data build on previous work in overweight men and women (8) reporting similar glucose and insulin postprandial responses after light- and moderate-intensity walking. The present findings extend these observations by suggesting that metabolic benefits are also accrued when regularly breaking up prolonged sitting by moving from a sitting to a stationary upright posture.
To date, four other studies have examined the acute effect of standing on postprandial glucose and insulin responses (12,13,30,31). Two of these found that breaking prolonged sitting with regular standing breaks had no impact on postprandial glucose (30,31) or insulin (30) in young healthy men. In contrast, alternating 30-min bouts of sitting and standing throughout the day has been shown to significantly reduce the iAUC between trial conditions for postprandial glucose (11% reduction compared with prolonged sitting) (12). A nonrandomized office-based study also found that glucose levels were reduced by 43% following an afternoon of standing compared with seated computer work (13). The fact that our study reported effects that were toward the upper end of those reported in previous studies, while using substantially smaller doses of standing, is likely to be driven by differences in sample characteristics and potentially the increased frequency in interruptions to prolonged sitting. Other studies have been conducted in groups that are broadly representative of the general population (age <50 years, BMI <30 kg/m2), whereas our participants were older with existing dysglycemia who represent those likely to be referred into diabetes prevention pathways. This is particularly important given the prominence of national and international strategies highlighting the need for identification and subsequent referral of individuals at high risk of type 2 diabetes (32,33).
Another novel finding was that reductions in glucose and insulin responses after the breaking up of prolonged sitting were maintained into the second observation day. Glucose remained 19% lower after the standing condition and 17% lower after the walking condition. Similarly, insulin remained 24% lower after the walking condition. These findings are consistent with a previous experimental study carried out in obese adults showing that a single bout of modest exercise (50% VO2 peak on a stationary cycle ergometer) increased insulin sensitivity into the next day (11). A similar study also demonstrated that the morning after a prolonged bout of sitting (17 h), participants exhibited a significant reduction (39%) in whole-body insulin action compared with upright light-intensity activity (10). Our findings indicate that an even lower activity stimulus (e.g., standing) may yield metabolic advantages for a minimum of 24 h.
The mechanisms underpinning the effects of standing and walking on glucose and insulin levels require further elucidation. Acute and chronic light-intensity physical activity training studies have consistently demonstrated improvements in markers of glycemic control in those with dysglycemia, with similar effects observed between light- and moderate-intensity exercise training regimes, when matched for total volume (34). However, it has not been established whether the specific mechanisms involved in enhancing peripheral glucose uptake that have been shown for MVPA, primarily through the translocation and turnover of GLUT4 (35), are observed with walking at a self-perceived light intensity or standing.
The attenuated postprandial suppression in plasma NEFA concentration observed on day 1 of this study for both the standing and walking is likely to reflect an increase in the lipolysis of triglycerides stored in adipose tissue in order to supply the working muscle. Moreover, the reduction of insulin in the standing and walking conditions suggests that suppression of lipolysis, driven by the antilipolytic properties of insulin (36), may have been reduced in these conditions. Previous studies have shown that during low-intensity exercise, adipose tissue lipolysis increases four- to fivefold above resting levels (37). Others have also reported that lipolysis and mobilization of NEFA resulting from exercise are related to, and may be enhanced by, hormonal changes, particularly increased catecholamines levels (38).
We found no change in the triglyceride iAUC for the standing and walking conditions on either day 1 or day 2 of the experimental regimens. The nonsignificant results on day 1 are consistent with previous studies that have shown no effect (9,12). Decreased triglyceride levels were observed on day 2 after the walking condition, although the changes were not statistically significant (17% reduction compared with sitting, P = 0.077). However, the magnitude of the effect for walking on day 2 was consistent with previous studies demonstrating that walking (both intermittent and continuous) elicited reductions in the postprandial triglyceride levels the following day (16–23% reduction). Our results corroborate with other findings suggesting that standing is not a sufficient stimulus to reduce postprandial triglyceride levels (12,30).
This study has a number of strengths. Firstly, we studied postmenopausal women at high risk of type 2 diabetes, so the findings are directly relevant for public health guidance and interventions for metabolic risk reduction. Secondly, this is the first study to directly compare the effects of breaking up prolonged sitting with standing and walking, demonstrating that they both induce cardiometabolic benefits. Moreover, by using a 2-day protocol we were able to determine that the acute effects of standing and walking persisted into the following day. Our study also highlights the importance of reporting both iAUC and total AUC in experimental studies that assess outcomes over several days. Although results on day 1 were unaffected by the analysis method, there were small differences in interpretation on day 2. Notwithstanding the nonsignificant differences in mean fasting levels on day 2, it is possible that the intervention conditions had a subtle effect on fasting pathophysiology that subsequently influenced total AUC. As such, results should be interpreted in relation to the method used; for this study, the primary focus was on the postprandial response (iAUC). Finally, all measurements were performed by the same team of trained staff, following identical standard operating procedures, and analysis was conducted by individuals blinded to treatment allocation.
This study has several important limitations. Firstly, the acute nature of the trial prohibits inferences about longer-term chronic effects. Secondly, the test meals used were relatively high in fat (58% of total energy), and further studies are needed to determine whether the findings persist when meals with a macronutrient composition more representative of dietary recommendations are consumed. However, the macronutrient composition of food was almost identical to that which may be plausibly consumed by the general population through a meal or as a snack. For example, based on an 80-kg individual, the standardized meal used in this study is equivalent to 46 g brown bread, 6 g butter, 100 g bacon, and a 59-g chocolate bar (39). Studies have also indicated that the recommended daily intake of fat is often exceeded by many adults (40). We also relied on participants to record and standardize their own food intake the day before and in between each experimental condition for practical reasons; therefore, misreporting is possible. Similarly, no physical activity data were recorded between day 1 and day 2. Thirdly, the prolonged nature of the sitting condition may not reflect habitual behavior for many individuals where some standing or light movement would be expected over an 8 h period. Nonetheless, it was important to initially establish a proof of concept where standing and walking effects are observed compared with a prolonged standardized bout of sitting. Future studies should also focus on whether the effects observed in this study are replicated under free-living scenarios. The reduced sample size (and subsequent underpowered comparison), particularly pertaining to comparisons on day 2, increased the risk of a type 2 error and thus limits the conclusions that can be drawn over the second day. Furthermore, the study was not designed to assess differences between the standing and walking conditions, which were included as a secondary outcome. Finally, further research is needed to determine whether the effects can be generalized to men and premenopausal women.
In conclusion, this study demonstrates that breaking up prolonged sitting with 5-min bouts of standing or walking at a self-perceived light intensity reduces postprandial glucose, insulin, and NEFA responses in postmenopausal women at high risk of type 2 diabetes. This simple, behavioral approach could inform future public health interventions aimed at improving the metabolic profile of dysglycemic individuals. Habitual standing and light-intensity physical activity are behaviorally more ubiquitous than MVPA and may therefore provide appealing interventional targets in the promotion of metabolic health. However, future behavioral intervention studies are needed to investigate the most effective methods of reducing habitual sedentary behavior within a prevention context and to assess generalizability beyond postmenopausal women.
Clinical trial reg. no. NCT02135172, clinicaltrials.gov.
Article Information
Acknowledgments. The authors thank Ros Downing, Steve Hartshorn, Carrie Wilson, Tim Skelton, Hamid Mani, David Webb, Zin Zin Htike, Sarah Bunnewell, Jo Paul, Balu Webb, Helen Waller, and Ellen Edwardson for their assistance throughout the study. A special thank you must also go to all participants who took the time to take part.
Funding. The research was supported by the National Institute for Health Research (NIHR) Leicester-Loughborough Diet, Lifestyle and Physical Activity Biomedical Research Unit, which is a partnership between University Hospitals of Leicester National Health Service Trust, Loughborough University, and the University of Leicester; NIHR Collaborations for Leadership in Applied Health Research and Care, Leicestershire, Northamptonshire, and Rutland (NIHR CLAHRC–LNR) and East Midlands (NIHR CLAHRC EM); and the University of Leicester Clinical Trials Unit.
The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, or the Department of Health.
Duality of Interest. M.J.D., T.Y., and K.K. (Chair) are members of the National Institute for Health and Care Excellence Public Health Guidance (PH38) Preventing type 2 diabetes: risk identification and interventions for individuals at high risk. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. J.H., M.J.D., D.H.B., C.L.E., J.M.R.G., D.J.S., K.T., D.W.D., K.K., and T.Y. made significant contributions to the concept and subsequent design of the study, made substantial contributions to analysis and interpretation, provided critical revision of the manuscript, and approved the final version of the manuscript. J.H. and T.Y. wrote the manuscript. J.H. supervised the study. J.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented at the International Diabetes Federation’s 2015 World Diabetes Congress, Vancouver, Canada, 30 November–4 December 2015.